1/
Have you ever wondered why advanced renal disease often leads to often debilitating pruritis?
Why would kidney failure lead someone to itch uncontrollably?
#tweetorial x.com
Have you ever wondered why advanced renal disease often leads to often debilitating pruritis?
Why would kidney failure lead someone to itch uncontrollably?
#tweetorial x.com
4/
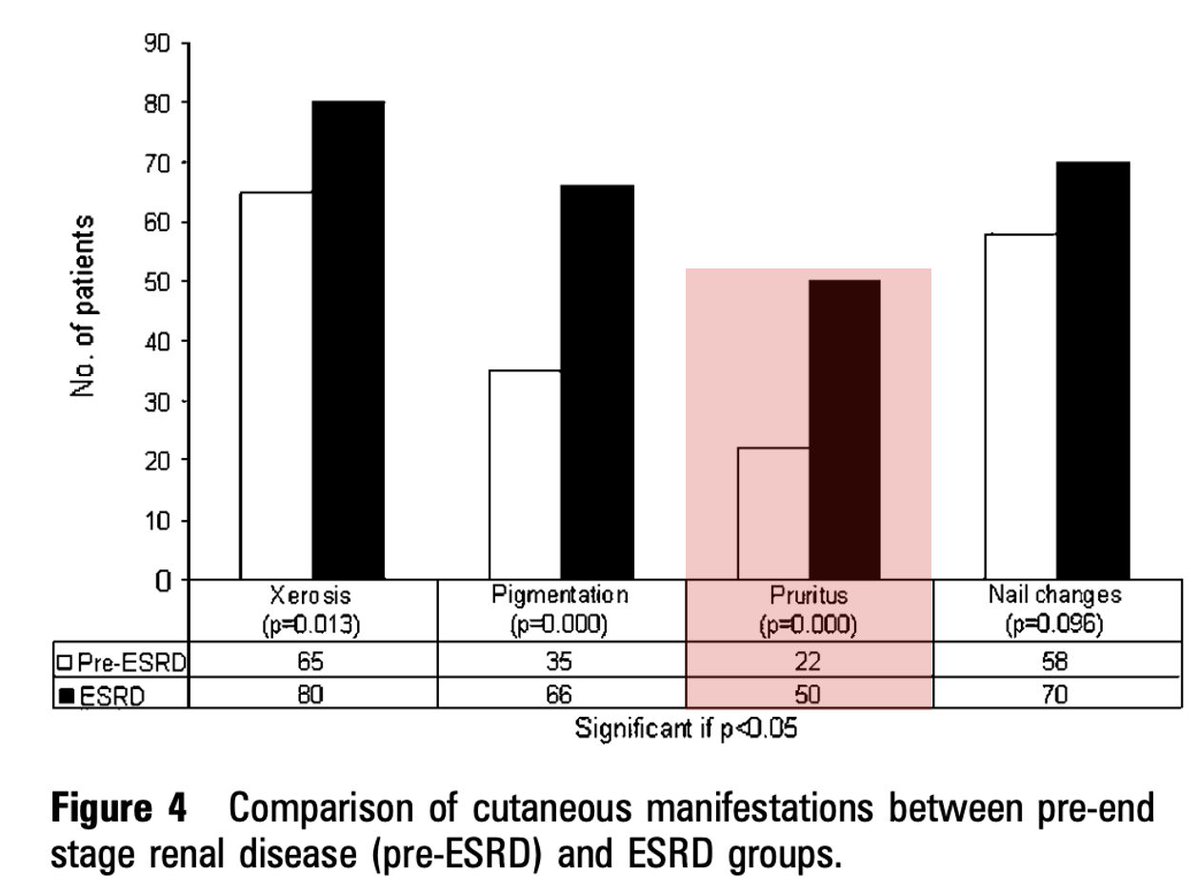
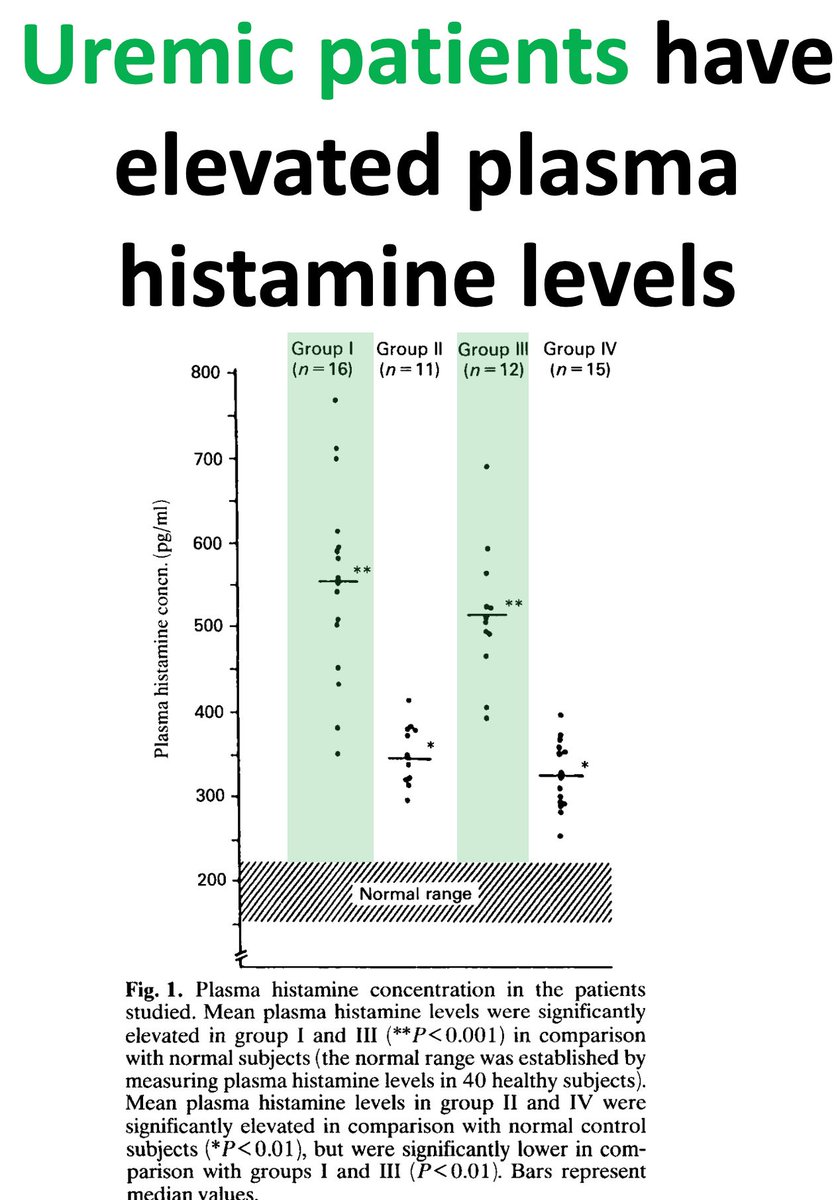
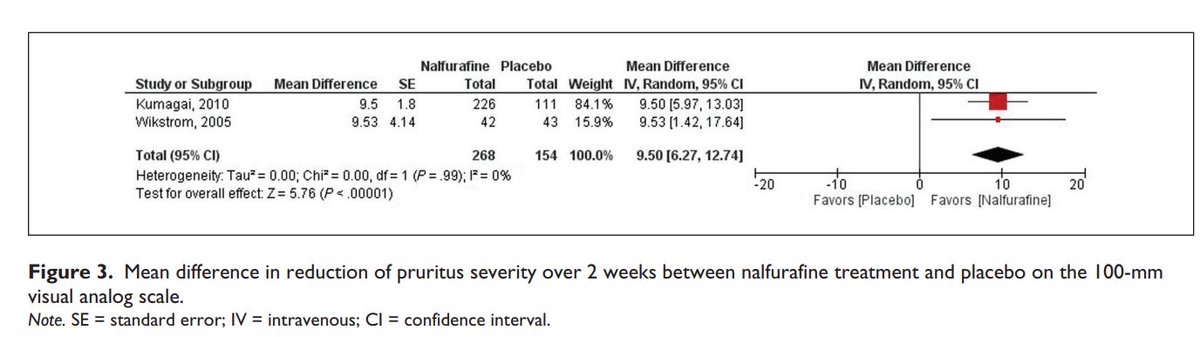
Uremic pruritis (UP) seems to be a Hickam's dictum-type situation, with more than one pathophysiologic cause.
The overall problem, not surprisingly, seems to relate to metabolic derangement from renal failure.
But why would that make someone itch so severely?
Uremic pruritis (UP) seems to be a Hickam's dictum-type situation, with more than one pathophysiologic cause.
The overall problem, not surprisingly, seems to relate to metabolic derangement from renal failure.
But why would that make someone itch so severely?
5/
The proposed pathophysiologic mechanisms for UP seem to break down along two broad categories: cutaneous/peripheral and systemic.
Let's start with cutaneous/peripheral.
buff.ly
The proposed pathophysiologic mechanisms for UP seem to break down along two broad categories: cutaneous/peripheral and systemic.
Let's start with cutaneous/peripheral.
buff.ly
10/
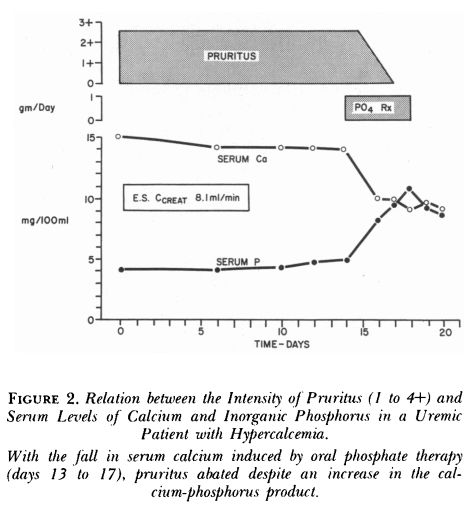
Related to hyperparathyroidism, elevated Ca may contribute to pruritis as well, possibly by subclinical precipitation within the skin.
buff.ly
Related to hyperparathyroidism, elevated Ca may contribute to pruritis as well, possibly by subclinical precipitation within the skin.
buff.ly
14/
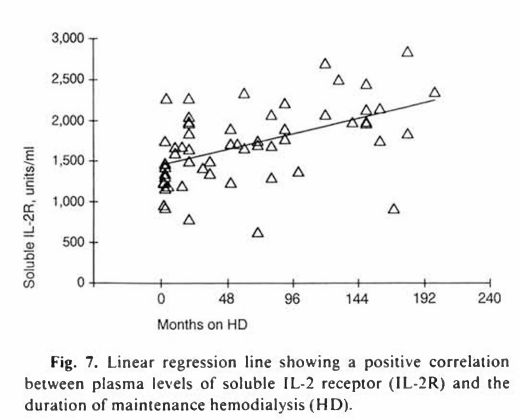
Some also have theorized that UP is an inflammatory condition, driven by T lymphocyte activation and cytokine production.
IL-2 offers an intriguing possible mechanistic explanation, as it can cause itchiness when injected into the skin.
buff.ly
Some also have theorized that UP is an inflammatory condition, driven by T lymphocyte activation and cytokine production.
IL-2 offers an intriguing possible mechanistic explanation, as it can cause itchiness when injected into the skin.
buff.ly
16/SUMMARY
Hopefully it's clear that uremic pruritis is very much multifactorial. But when thinking about causes, local/cutaneous vs. systemic etiologies may be a helpful framework.
Itch scratched!
Hopefully it's clear that uremic pruritis is very much multifactorial. But when thinking about causes, local/cutaneous vs. systemic etiologies may be a helpful framework.
Itch scratched!
جاري تحميل الاقتراحات...