(1/x) The inferior vena cava (IVC) is 'useless' is a phrase stated confidently and incorrectly by #pocus novices. ❌
The IVC is useless at:
- telling you what to eat for dinner
- acting as a fuel gauge for volume status
- predicting fluid responsiveness
HOWEVER.
The IVC is incredibly useful in helping us decide on the optimal fluid and decongestion strategy for your patients.
A 🧵
(With a bonus discussion of future of #VEXUS research at the end. )
#medtwitter #foamed #echofirst
The IVC is useless at:
- telling you what to eat for dinner
- acting as a fuel gauge for volume status
- predicting fluid responsiveness
HOWEVER.
The IVC is incredibly useful in helping us decide on the optimal fluid and decongestion strategy for your patients.
A 🧵
(With a bonus discussion of future of #VEXUS research at the end. )
#medtwitter #foamed #echofirst
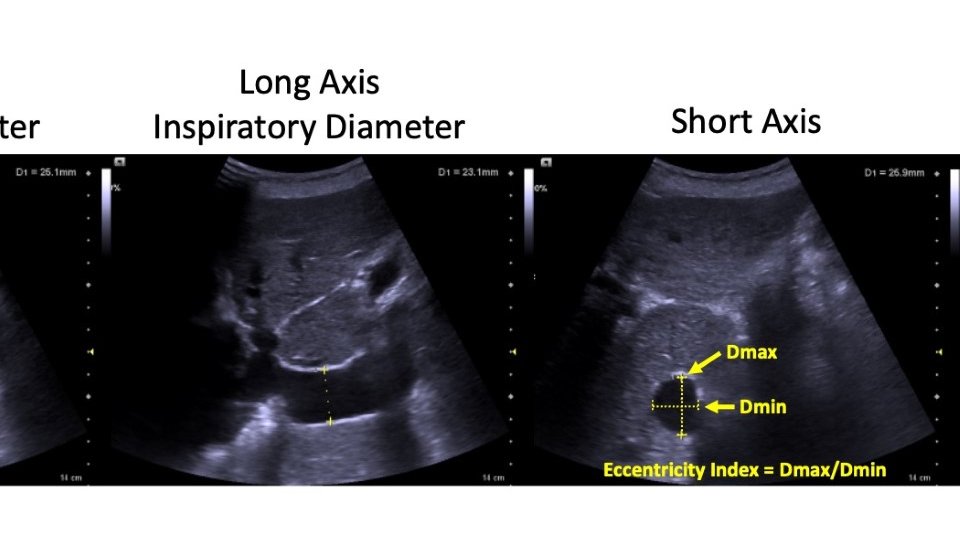
(2/x) When we talk about IVC size and collapsibility thresholds, people often cite 2cm or 50% as the magic threshold.
These are irrelevant for almost everything.
The cutoffs were derived and explored as a surrogate for CVP and for thresholds to predict fluid responsiveness.
IVC does not predict fluid responsiveness, and using IVC to predict static CVP (as we will see) is useless because organ level Doppler is more predictive of congestion.
Instead, I try to think of where on the spectrum from fully collapsed IVC to fully plethoric it lies (considering short axis and long axis for as much of the intrahepatic IVC as possible).
You can have severe venous congestion with an IVC of 1.5 cm and no venous congestion with an IVC of 4cm.
These are irrelevant for almost everything.
The cutoffs were derived and explored as a surrogate for CVP and for thresholds to predict fluid responsiveness.
IVC does not predict fluid responsiveness, and using IVC to predict static CVP (as we will see) is useless because organ level Doppler is more predictive of congestion.
Instead, I try to think of where on the spectrum from fully collapsed IVC to fully plethoric it lies (considering short axis and long axis for as much of the intrahepatic IVC as possible).
You can have severe venous congestion with an IVC of 1.5 cm and no venous congestion with an IVC of 4cm.
(3/x) When someone says 'the IVC assessment on #POCUS is useless' - this is a good indicator they only have a surface understanding of POCUS.
If you ask the IVC what to grab for dinner - it will be useless at that.
If you ask the IVC where you should vacation with your family - also useless
If you ask the IVC about fluid responsiveness - useless.
If you ask the IVC about fluid tolerance and venous congestion - useful!!!
But remember, similar to other veins, the IVC is not round. Interrogating the IVC only in long axis ignores this fact. I try to interrogate the entire intrahepatic IVC in long and short axis to get a general gestalt of degree of distension.
If you ask the IVC what to grab for dinner - it will be useless at that.
If you ask the IVC where you should vacation with your family - also useless
If you ask the IVC about fluid responsiveness - useless.
If you ask the IVC about fluid tolerance and venous congestion - useful!!!
But remember, similar to other veins, the IVC is not round. Interrogating the IVC only in long axis ignores this fact. I try to interrogate the entire intrahepatic IVC in long and short axis to get a general gestalt of degree of distension.
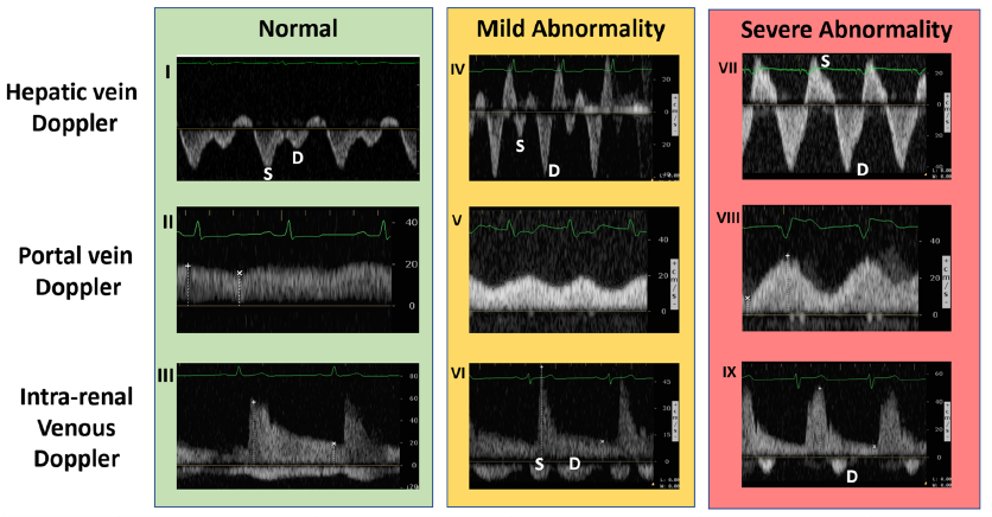
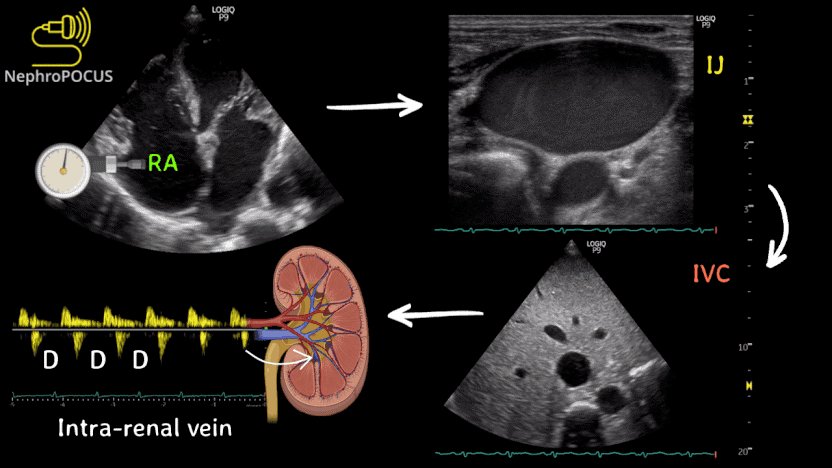
(4/x) Venous congestion is a pathologic state where high venous pressures are transmitted retrograde from the right atria into organs like the liver, brain, kidney, and bowel causing organ dysfunction.
CVP predicts venous congestion, but only weakly.
#VEXUS or #Doppler markers of congestion are better predictors of venous congestion.
IVC certainly has some role in this too - for patients with a totally collapsed IVC, they are less like to have venous congestion. For patients with a severely distended IVC, they are more likely.
This however, (like CVP) is actually imprecise at a patient level with only moderate predictive accuracy, which is why #VEXUS uses organ level Doppler of the hepatic vein, portal vein, and intra-renal vein to predict fluid responsiveness
CVP predicts venous congestion, but only weakly.
#VEXUS or #Doppler markers of congestion are better predictors of venous congestion.
IVC certainly has some role in this too - for patients with a totally collapsed IVC, they are less like to have venous congestion. For patients with a severely distended IVC, they are more likely.
This however, (like CVP) is actually imprecise at a patient level with only moderate predictive accuracy, which is why #VEXUS uses organ level Doppler of the hepatic vein, portal vein, and intra-renal vein to predict fluid responsiveness
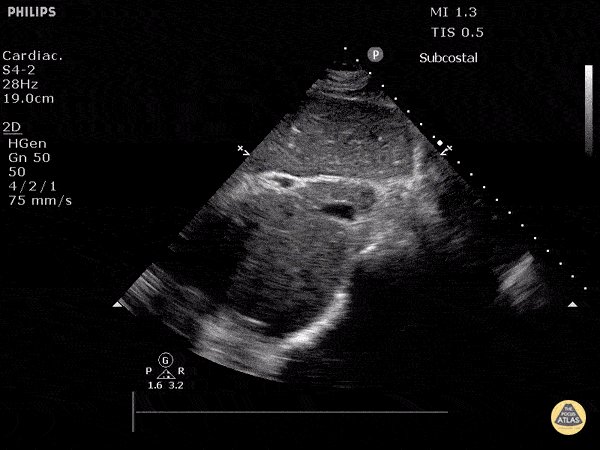
(5/x) So how do I use IVC in practice?
If I see a totally collapsed IVC (tiny + 100% collapsible) I think venous congestion from a central cause (high RA pressure) is unlikely.
When I see a mid-range or distended IVC, when I am concerned clinically for congestion induced organ injury, that invites me to interrogate the end organs themselves to see if that elevated pressure may be transmitted retrograde.
@ArgaizR has some interesting data on this, but essentially, it is rare to have severe venous congestion with a totally collapsed IVC.
Credit to @NephroP for this great diagram and if you want to learn more about congestion, nephropocus.com is probably the best resource out there!!!
If I see a totally collapsed IVC (tiny + 100% collapsible) I think venous congestion from a central cause (high RA pressure) is unlikely.
When I see a mid-range or distended IVC, when I am concerned clinically for congestion induced organ injury, that invites me to interrogate the end organs themselves to see if that elevated pressure may be transmitted retrograde.
@ArgaizR has some interesting data on this, but essentially, it is rare to have severe venous congestion with a totally collapsed IVC.
Credit to @NephroP for this great diagram and if you want to learn more about congestion, nephropocus.com is probably the best resource out there!!!
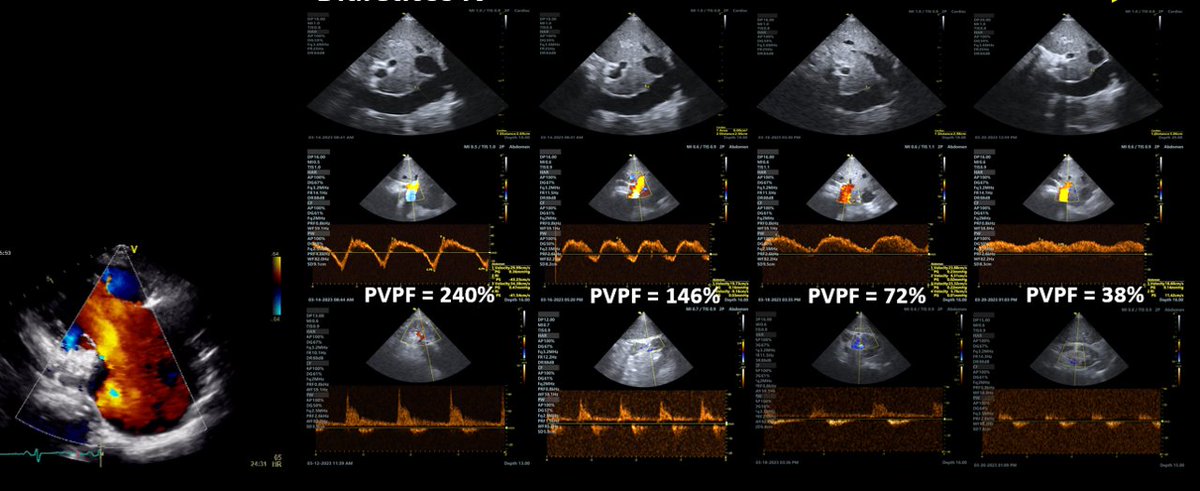
(6/x) So is the #VEXUS score in its purest form still valid? (i.e. the original paper by @WBeaubien @ThinkingCC et al.)
Conceptually, absolutely.
Do the exact thresholds and cutoffs used in the original scoring system apply perfectly to all populations? No.
VEXUS was derived and validated primarily in a cardiac surgical population, with increasing number of studies in other populations assessing and validating it.
With that said, however, the thresholds by which congestion cause organ dysfunction depend on the cause of the congestion.
For example, severe TR related congestion will always have an abnormal hepatic vein, however, with decongestion, portal vein pulsatility can normalize.
Similarly, PV pulsatility in pulmonary HTN patients does not typically normalize to less than 50% so normal for one of those patients could be >50% which traditionally would be severe congestion.
Credit to @ArgaizR for the diagram.
Conceptually, absolutely.
Do the exact thresholds and cutoffs used in the original scoring system apply perfectly to all populations? No.
VEXUS was derived and validated primarily in a cardiac surgical population, with increasing number of studies in other populations assessing and validating it.
With that said, however, the thresholds by which congestion cause organ dysfunction depend on the cause of the congestion.
For example, severe TR related congestion will always have an abnormal hepatic vein, however, with decongestion, portal vein pulsatility can normalize.
Similarly, PV pulsatility in pulmonary HTN patients does not typically normalize to less than 50% so normal for one of those patients could be >50% which traditionally would be severe congestion.
Credit to @ArgaizR for the diagram.
(7/x) So what is the future of congestion research in my opinion? Understanding endotypes of congestion and disease specific patterns.
I think the next big step in venous congestion research is understanding endotypes of congestion, or specific patterns relevant to different populations of congested patients and different causes.
For example, how is tricuspid regurgitation associated congestion similar and different to RV failure associated congestion.
Also, for different populations, is the threshold that congestion causes injury for septic patients the same as cardiac surgical? (when different physiological status).
Lots to discover, but exciting times ahead!
I think the next big step in venous congestion research is understanding endotypes of congestion, or specific patterns relevant to different populations of congested patients and different causes.
For example, how is tricuspid regurgitation associated congestion similar and different to RV failure associated congestion.
Also, for different populations, is the threshold that congestion causes injury for septic patients the same as cardiac surgical? (when different physiological status).
Lots to discover, but exciting times ahead!
جاري تحميل الاقتراحات...