Idiopathic intracranial hypertension (IIH)
This relatively common disorder is an important secondary cause of headache and can cause permanent vision loss. Let’s dive into the presentation, work up, and diagnosis together!
#neurology #FOAMed #MedEd #neurotwitter #tweetorial
This relatively common disorder is an important secondary cause of headache and can cause permanent vision loss. Let’s dive into the presentation, work up, and diagnosis together!
#neurology #FOAMed #MedEd #neurotwitter #tweetorial
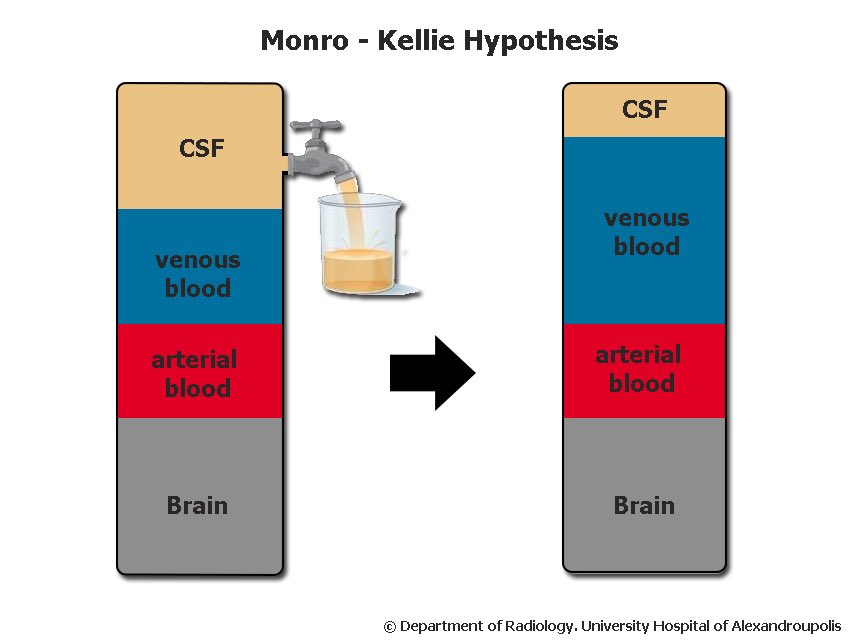
IIH is a syndrome characterized by CSF hypertension which is not due to obstruction or other mass-occupying lesion.
The prevalence is about 1 in 100,000 in the general population, but it’s 20 times more common in the highest risk population, obese women < 45.
The prevalence is about 1 in 100,000 in the general population, but it’s 20 times more common in the highest risk population, obese women < 45.
Risk factors for IIH include:
- female sex
- age 15-44
- obesity
- sleep apnea
- certain meds (eg vitamin A analogs, tetracyclines)
- venous sinus stenosis (primary or secondary)
- female sex
- age 15-44
- obesity
- sleep apnea
- certain meds (eg vitamin A analogs, tetracyclines)
- venous sinus stenosis (primary or secondary)
Symptoms:
- Headache (esp “reverse orthostatic” HA worse when laying down or in the morning)
- Pulsatile tinnitus
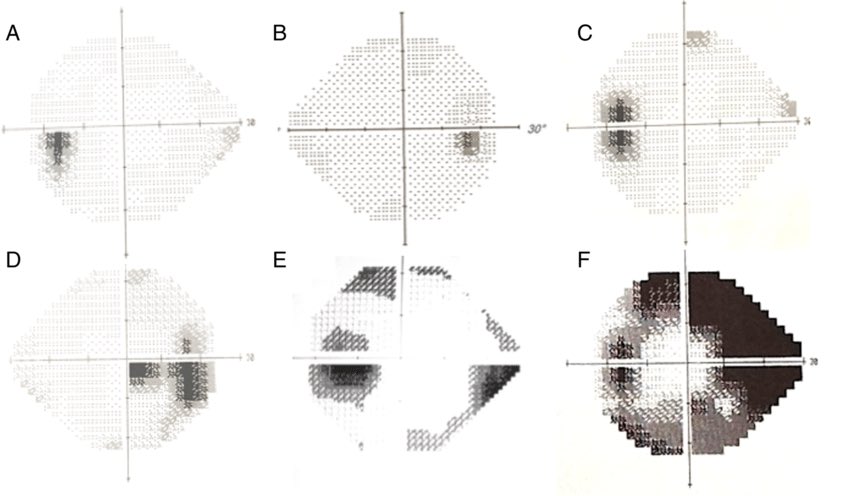
- Visual symptoms
> Transient visual obscurations
(particularly w/ Valsalva)
> Photopsia
> Visual field constriction
- Headache (esp “reverse orthostatic” HA worse when laying down or in the morning)
- Pulsatile tinnitus
- Visual symptoms
> Transient visual obscurations
(particularly w/ Valsalva)
> Photopsia
> Visual field constriction
Diagnosis is based on the modified Dandy criteria, essentially requiring:
- Signs and symptoms of IIH
- No mass occupying lesion or other 1:1 cause of intracranial hypertension
- Elevated CSF opening pressure
- Signs and symptoms of IIH
- No mass occupying lesion or other 1:1 cause of intracranial hypertension
- Elevated CSF opening pressure
Work up will require:
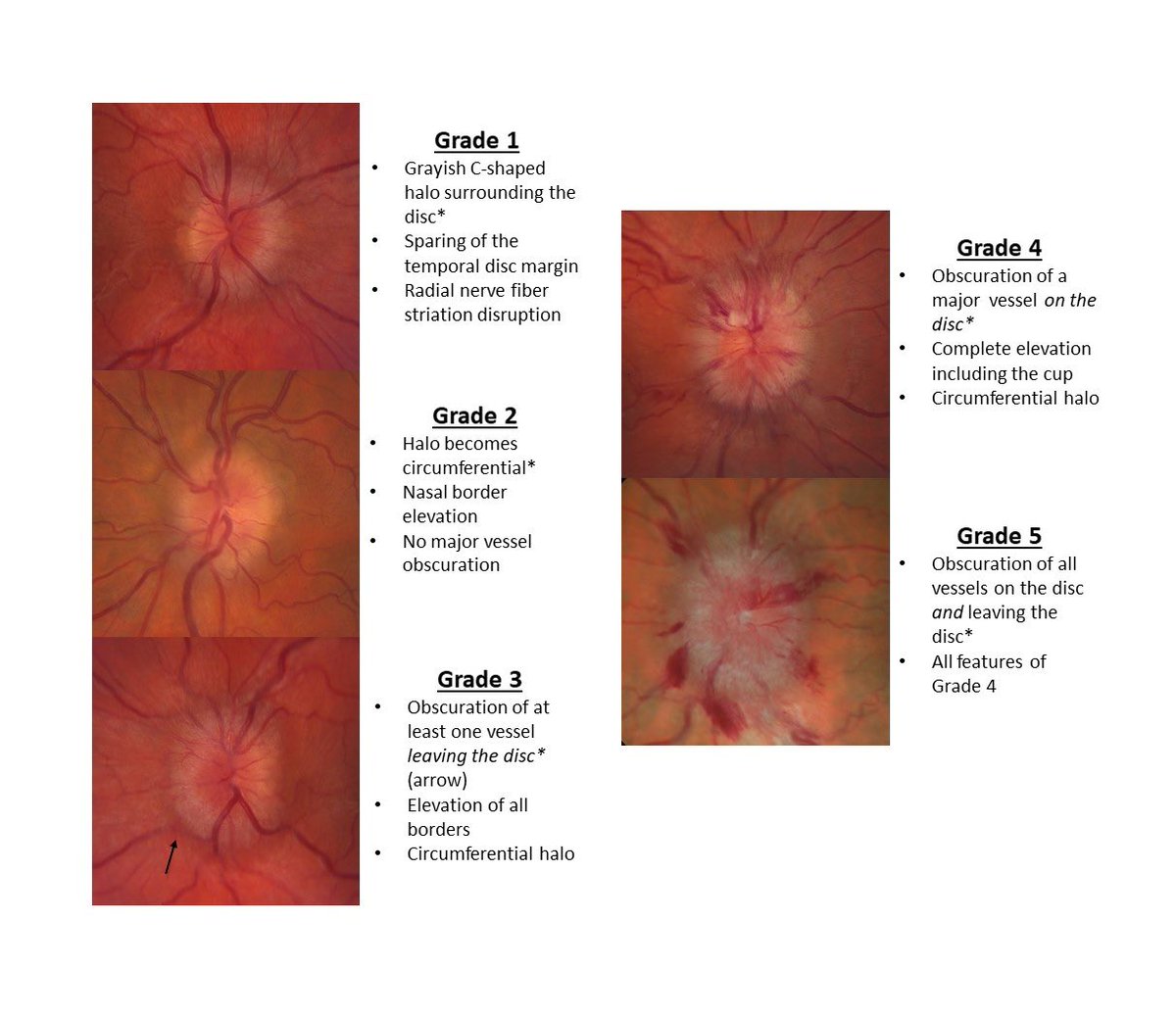
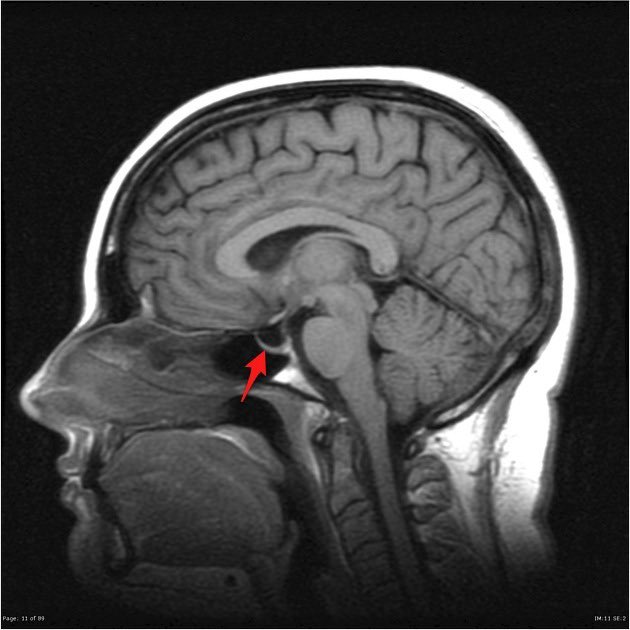
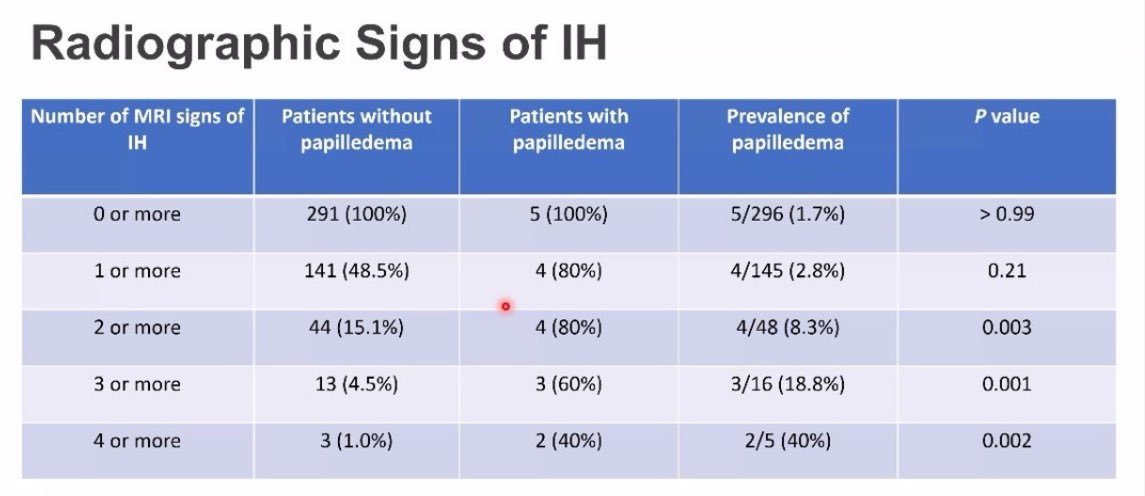
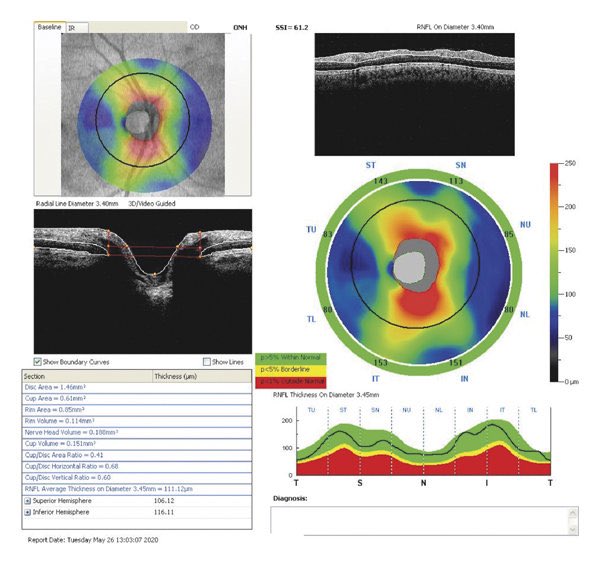
- MRI imaging to exclude tumor, venous sinus thrombus, and other structural causes of intracranial hypertension
- LP with opening pressure to demonstrate CSF hypertension and exclude meningitis or CNS inflammation
- MRI imaging to exclude tumor, venous sinus thrombus, and other structural causes of intracranial hypertension
- LP with opening pressure to demonstrate CSF hypertension and exclude meningitis or CNS inflammation
TREATMENT
The feared outcome of IIH is vision loss, so treatment revolves around preventing this. Treatment of other symptoms like headache and tinnitus are important but secondary goals.
The feared outcome of IIH is vision loss, so treatment revolves around preventing this. Treatment of other symptoms like headache and tinnitus are important but secondary goals.
Addressing risk factors such as untreated sleep apnea, weight loss in the case of obesity, and cessation of offending meds should be our very first step.
First line medical treatment is with carbonic anhydrase inhibitors. This generally means acetazolamide, although topiramate has emerged as a potentially equally effective treatment which additionally helpful in treating headaches.
Second-line options include loop diuretics.
Second-line options include loop diuretics.
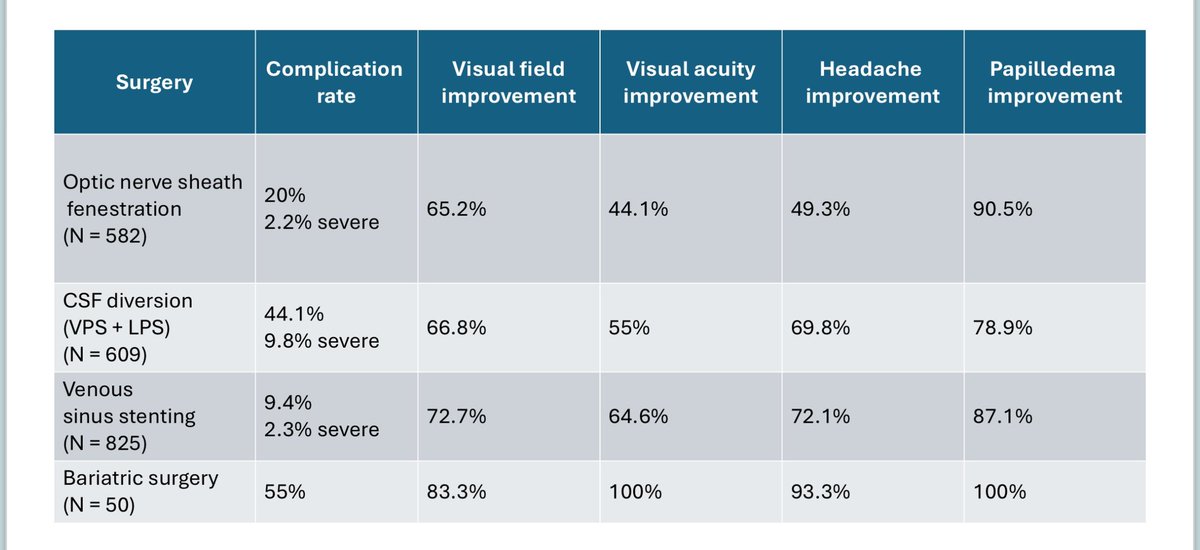
Surgery is generally reserved for refractory cases or for those with advanced or rapidly progressive vision loss.
There are four surgical options: optic nerve sheath fenestration, CSF diversion (shunting), venous sinus stenting, and bariatric surgery.
There are four surgical options: optic nerve sheath fenestration, CSF diversion (shunting), venous sinus stenting, and bariatric surgery.
CSF shunting has fallen out of favor recently, having a much higher complication rate and equivalent efficacy. Venous sinus stenosis is emerging as a more popular surgical approach and has similar quality of supportive data as the other surgical treatments.
Take-home points:
- IIH is relatively common and requires MRI and LP to diagnose
- Incidental IIH-like findings are very common; look for symptoms and multiple findings
- First line treatment is with risk factor management and acetazolamide
- Ongoing monitoring is crucial
- IIH is relatively common and requires MRI and LP to diagnose
- Incidental IIH-like findings are very common; look for symptoms and multiple findings
- First line treatment is with risk factor management and acetazolamide
- Ongoing monitoring is crucial
جاري تحميل الاقتراحات...