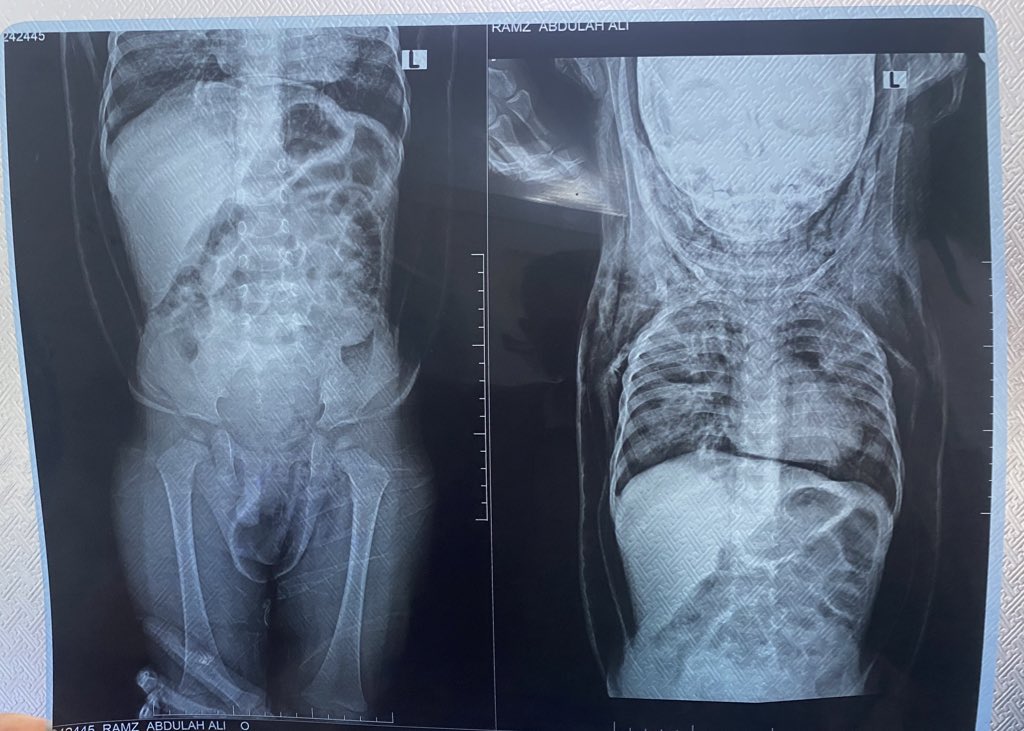
A 2-y-o male pt with a Hx of hospitalization for pneumonia suddenly presents with generalized body swelling and severe respiratory distress.There is no Hx of trauma.On PE,crepitus is noted when the swollen areas are palpated.
What is the cause of deterioration in this case?
What’s the diagnosis?
#Findings ?
#MedX #MedTwitter #MEDHM @IhabFathiSulima
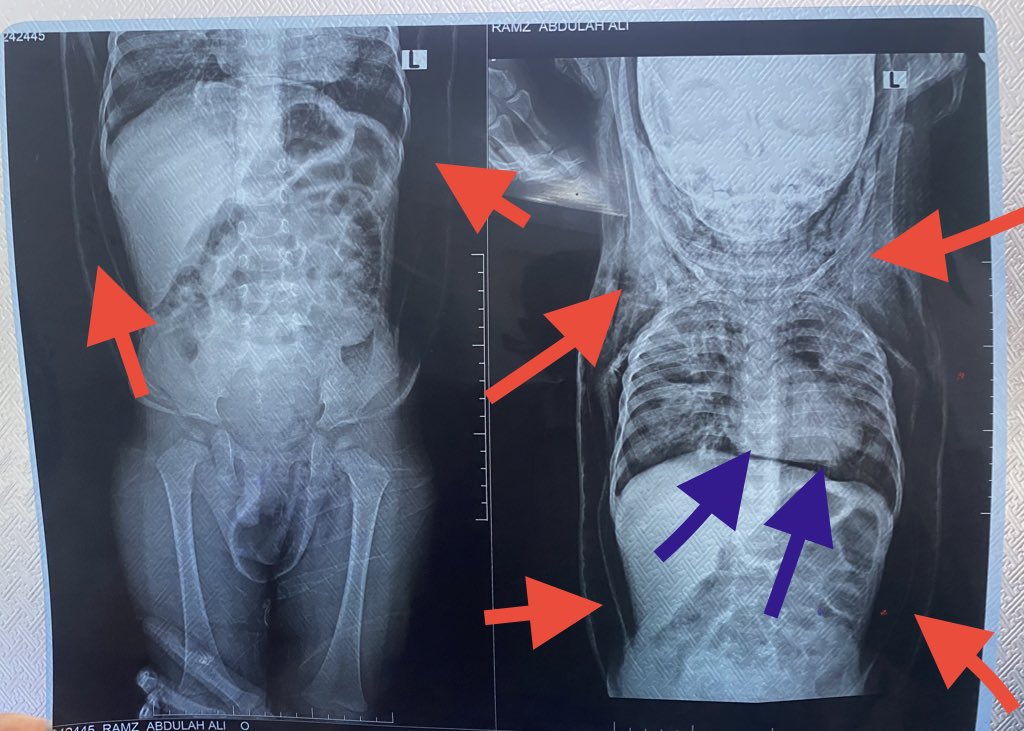
What is the cause of deterioration in this case?
What’s the diagnosis?
#Findings ?
#MedX #MedTwitter #MEDHM @IhabFathiSulima
#Answer :
Patient with history of generalized body swelling and subcutaneous crepitu suspected emphysema,
the #imaging_findings show:
• Severe pneumomediastinum(green arrows) assoicated with severe chest wall emphysema extend to the neck and down to the abdomen (red arrows)
with patchy area of consolidation and ground glass attenuation affecting the right upper lung lobe , right lower lung lobe, left upper lobe
#Diagnosis:
-The above-mentioned
findings keeping with severe
#pneumomediastinum,diffuse
#soft_tissue_emphysema of the neck, chest and abdomen.Patchy area of consolidation of both lungs (likely infection Or contusion).
#MedTwitter #MEDHM #MedX @IhabFathiSulima
Patient with history of generalized body swelling and subcutaneous crepitu suspected emphysema,
the #imaging_findings show:
• Severe pneumomediastinum(green arrows) assoicated with severe chest wall emphysema extend to the neck and down to the abdomen (red arrows)
with patchy area of consolidation and ground glass attenuation affecting the right upper lung lobe , right lower lung lobe, left upper lobe
#Diagnosis:
-The above-mentioned
findings keeping with severe
#pneumomediastinum,diffuse
#soft_tissue_emphysema of the neck, chest and abdomen.Patchy area of consolidation of both lungs (likely infection Or contusion).
#MedTwitter #MEDHM #MedX @IhabFathiSulima
#Pneumomediastinum:
Definition: Pneumomediastinum is the presence of air in the mediastinum, the central compartment of the thoracic cavity.
#Etiology:
•Spontaneous Pneumomediastinum: Often results from alveolar rupture, where air escapes into the mediastinum. It can occur in conditions like asthma, vigorous coughing, vomiting, or heavy lifting.
•Traumatic Pneumomediastinum: Caused by chest trauma, esophageal or tracheal injury, or medical procedures such as endoscopy or mechanical ventilation.
•Infectious Pneumomediastinum: Rare, but can occur with gas-producing organisms in mediastinitis.
#Pathophysiology:
•Alveolar rupture allows air to dissect along the bronchovascular bundles into the mediastinum (Macklin effect).
•Air can also originate from other sources like the esophagus, trachea, or cervical soft tissues.
#Clinical_Features:
•Symptoms: Chest pain (retrosternal), dyspnea, neck pain, dysphagia, and voice changes.
•Signs: Subcutaneous emphysema, Hamman’s sign (a crunching sound synchronous with the heartbeat), and rarely, cardiovascular collapse if severe.
#Diagnosis:
•Imaging: Chest X-ray or CT scan showing air in the mediastinum.
•Additional Tests: Esophagram or bronchoscopy if esophageal or tracheal injury is suspected.
#Management:
•Observation: Many cases are self-limiting and resolve spontaneously, especially if there is no underlying severe pathology.
•Oxygen Therapy: High-flow oxygen can hasten the reabsorption of mediastinal air.
•Treatment of Underlying Cause: For example, antibiotics if infection is suspected or surgery if there’s a tracheal or esophageal rupture.
•Monitoring: Close clinical and imaging follow-up to ensure no progression or complications.
#MEDHM #MedEd #MedTwitter #MedX @IhabFathiSulima
Definition: Pneumomediastinum is the presence of air in the mediastinum, the central compartment of the thoracic cavity.
#Etiology:
•Spontaneous Pneumomediastinum: Often results from alveolar rupture, where air escapes into the mediastinum. It can occur in conditions like asthma, vigorous coughing, vomiting, or heavy lifting.
•Traumatic Pneumomediastinum: Caused by chest trauma, esophageal or tracheal injury, or medical procedures such as endoscopy or mechanical ventilation.
•Infectious Pneumomediastinum: Rare, but can occur with gas-producing organisms in mediastinitis.
#Pathophysiology:
•Alveolar rupture allows air to dissect along the bronchovascular bundles into the mediastinum (Macklin effect).
•Air can also originate from other sources like the esophagus, trachea, or cervical soft tissues.
#Clinical_Features:
•Symptoms: Chest pain (retrosternal), dyspnea, neck pain, dysphagia, and voice changes.
•Signs: Subcutaneous emphysema, Hamman’s sign (a crunching sound synchronous with the heartbeat), and rarely, cardiovascular collapse if severe.
#Diagnosis:
•Imaging: Chest X-ray or CT scan showing air in the mediastinum.
•Additional Tests: Esophagram or bronchoscopy if esophageal or tracheal injury is suspected.
#Management:
•Observation: Many cases are self-limiting and resolve spontaneously, especially if there is no underlying severe pathology.
•Oxygen Therapy: High-flow oxygen can hasten the reabsorption of mediastinal air.
•Treatment of Underlying Cause: For example, antibiotics if infection is suspected or surgery if there’s a tracheal or esophageal rupture.
•Monitoring: Close clinical and imaging follow-up to ensure no progression or complications.
#MEDHM #MedEd #MedTwitter #MedX @IhabFathiSulima
Soft Tissue Emphysema:
#Subcutaneous_emphysema
Definition: The presence of air in the soft tissues, usually the subcutaneous tissue. It often accompanies pneumomediastinum or pneumothorax.
#Etiology:
•Trauma: Blunt or penetrating injuries, fractures, or surgical procedures can introduce air into the soft tissues.
•Infections: Certain infections, especially those caused by gas-forming bacteria, can lead to soft tissue emphysema.
•Iatrogenic Causes: Procedures such as tracheostomy, chest tube insertion, or dental work can cause air to enter soft tissues.
#Pathophysiology:
•Air dissects along fascial planes from the mediastinum or pleural space into the subcutaneous tissue, often seen as swelling or crepitus upon palpation.
#Clinical_Features:
•Symptoms: May include swelling, pain, and a feeling of fullness or tightness in the affected area.
•Signs: Subcutaneous crepitus (a crackling sound when pressing on the skin), swelling, and possible skin discoloration.
#Diagnosis:
•Imaging: X-ray or CT can confirm the presence and extent of air in soft tissues. The pattern and distribution can help determine the source.
•Clinical Examination: Detection of crepitus on physical examination is often the first clue.
#Management:
•Treat the Underlying Cause: For example, managing a pneumothorax or addressing the source of trauma or infection.
•Observation: If mild and not progressing, it can often be managed conservatively.
•Surgical Intervention: Rarely, surgery may be needed to evacuate large amounts of air or address the underlying cause (e.g., repair of tracheal or esophageal injury).
•Antibiotics: If associated with an infection, particularly if there’s a risk of necrotizing fasciitis or other severe infections.
#MedTwitter #MEDHM #MedX @IhabFathiSulima
#Subcutaneous_emphysema
Definition: The presence of air in the soft tissues, usually the subcutaneous tissue. It often accompanies pneumomediastinum or pneumothorax.
#Etiology:
•Trauma: Blunt or penetrating injuries, fractures, or surgical procedures can introduce air into the soft tissues.
•Infections: Certain infections, especially those caused by gas-forming bacteria, can lead to soft tissue emphysema.
•Iatrogenic Causes: Procedures such as tracheostomy, chest tube insertion, or dental work can cause air to enter soft tissues.
#Pathophysiology:
•Air dissects along fascial planes from the mediastinum or pleural space into the subcutaneous tissue, often seen as swelling or crepitus upon palpation.
#Clinical_Features:
•Symptoms: May include swelling, pain, and a feeling of fullness or tightness in the affected area.
•Signs: Subcutaneous crepitus (a crackling sound when pressing on the skin), swelling, and possible skin discoloration.
#Diagnosis:
•Imaging: X-ray or CT can confirm the presence and extent of air in soft tissues. The pattern and distribution can help determine the source.
•Clinical Examination: Detection of crepitus on physical examination is often the first clue.
#Management:
•Treat the Underlying Cause: For example, managing a pneumothorax or addressing the source of trauma or infection.
•Observation: If mild and not progressing, it can often be managed conservatively.
•Surgical Intervention: Rarely, surgery may be needed to evacuate large amounts of air or address the underlying cause (e.g., repair of tracheal or esophageal injury).
•Antibiotics: If associated with an infection, particularly if there’s a risk of necrotizing fasciitis or other severe infections.
#MedTwitter #MEDHM #MedX @IhabFathiSulima
جاري تحميل الاقتراحات...