1) Welcome to a 🆕 #accredited #tweetorial on #Albuminuria: The Canary in the Coal Mine of #Kidney and #Cardiorenal #Disease. Our returning expert author is the wonderful teacher Edgar V. Lerma 🇵🇭 @edgarvlermamd
#Cardiorenal #Nephpearls #nephtwitter #FOAMed #CardioTwitter
#Cardiorenal #Nephpearls #nephtwitter #FOAMed #CardioTwitter
2) The program is intended for #HCPs & is supported by an independent educational grant from Bayer. Statement of accreditation and faculty disclosures at ckd-ce.com.
Follow this 🧵for 0.75hr 🆓 CE/#CME credit--all delivered right here on X!
Follow this 🧵for 0.75hr 🆓 CE/#CME credit--all delivered right here on X!
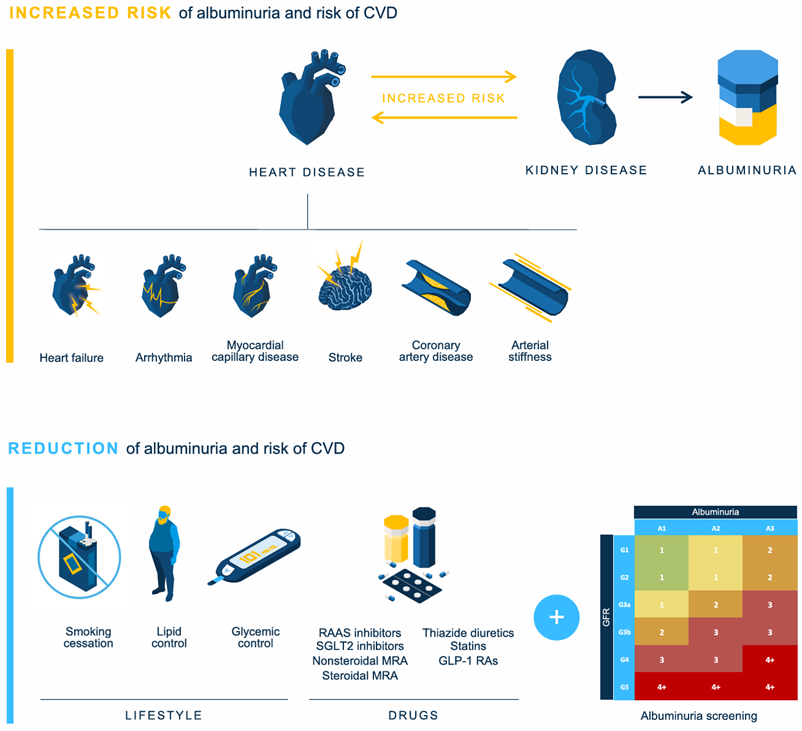
4) Let us extend this metaphor into #cardiorenal physiology and disease by looking at the cross talk between the heart and the kidneys
🔓 pubmed.ncbi.nlm.nih.gov
🔓 pubmed.ncbi.nlm.nih.gov
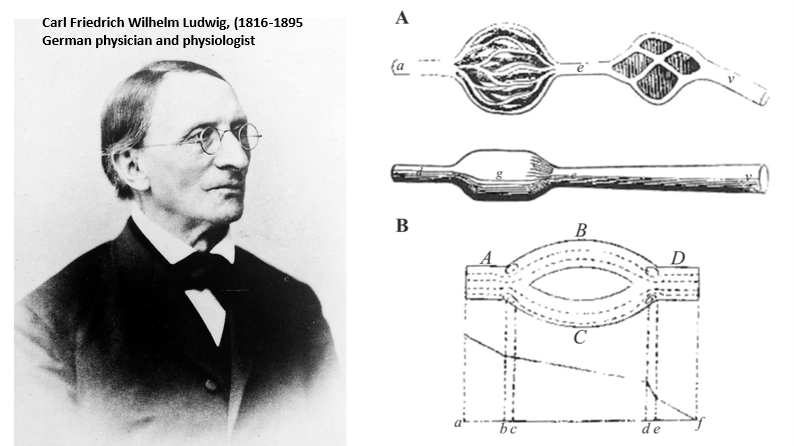
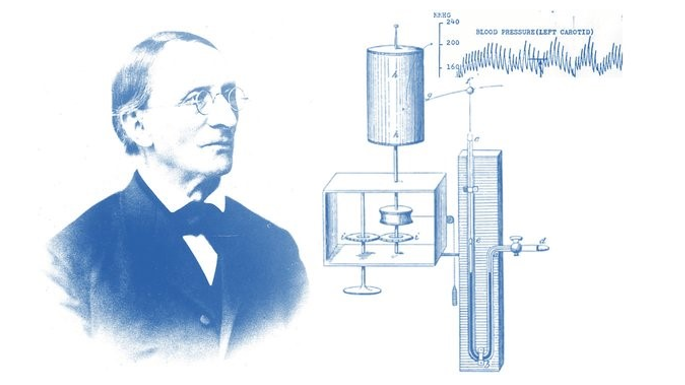
5a) In 1842, Carl F. W. Ludwig proposed the hypothesis that the urine is the result of a filtration process by the #glomeruli promoted by the force of blood pressure
🔓 pubmed.ncbi.nlm.nih.gov
🔓 pubmed.ncbi.nlm.nih.gov
5b) He further postulated that the final composition of the urine is the result of resorption processes taking place in the renal tubuli located downstream of the renal glomeruli
5c) Thus, the interplay of cardiac function (blood pressure) and kidney function (urine production) was described for the first time
🔓 pubmed.ncbi.nlm.nih.gov
🔓 pubmed.ncbi.nlm.nih.gov
5d) His work was published at a time when the physiological role of the kidneys was still being debated
At that time, a natural force (rather than #bloodpressure) was thought to be the driving force for urine production
🔓 pubmed.ncbi.nlm.nih.gov
At that time, a natural force (rather than #bloodpressure) was thought to be the driving force for urine production
🔓 pubmed.ncbi.nlm.nih.gov
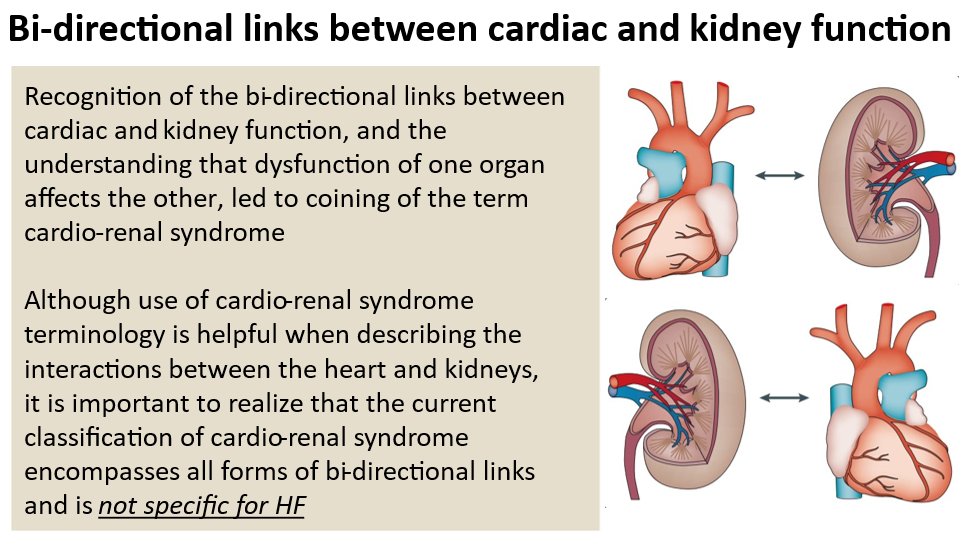
6b) Likewise, as a result of less glomerular filtration, the ensuing hypervolemia may lead to acute heart failure or aggravate a chronic heart failure (#CHF) condition
Thus, the heart and kidneys are both functionally dependent on each other
🔓 pubmed.ncbi.nlm.nih.gov
Thus, the heart and kidneys are both functionally dependent on each other
🔓 pubmed.ncbi.nlm.nih.gov
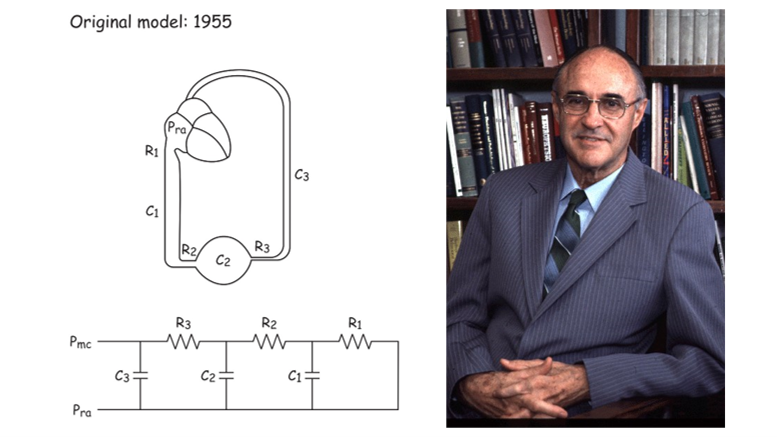
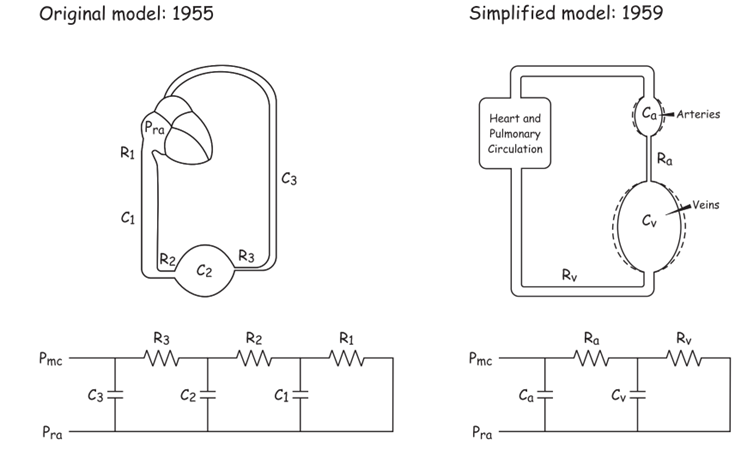
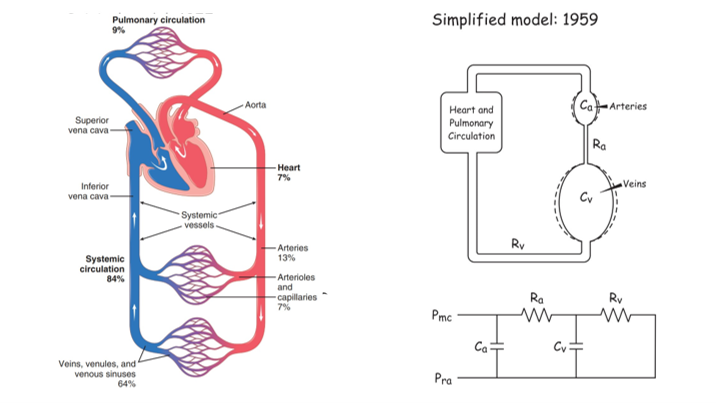
7a) 100 years later, Arthur C. Guyton described #cardiorenal syndrome #CRS as a combined cardiac and kidney dysfunction aggravating the failure of both organs progressively
🔓pubmed.ncbi.nlm.nih.gov
🔓pubmed.ncbi.nlm.nih.gov
7b) Guyton contributed physiological research on the role of the peripheral circulation to blood pressure regulation, which, in turn, affects kidney function
🔓 pubmed.ncbi.nlm.nih.gov
🔓 pubmed.ncbi.nlm.nih.gov
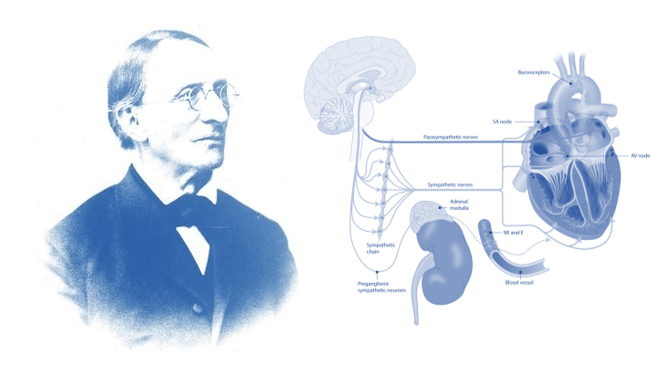
7c) However, it is to Carl Ludwig’s credit that afferent autonomic innervation such as the aortic depressor nerve is seen in the context of circulatory control
In fact, Ludwig proved that the aortic depressor nerve enters the brain stem, affecting blood pressure regulation
In fact, Ludwig proved that the aortic depressor nerve enters the brain stem, affecting blood pressure regulation
7d) Thus, Carl Ludwig’s work laid the basis for further research on the autonomic control of circulation
🔓 pubmed.ncbi.nlm.nih.gov
🔓 pubmed.ncbi.nlm.nih.gov
8a) During the last five decades, #neurohumoral stimulation including sympathetic activation, oxidative stress, and microinflammation have been proposed as pathomechanisms in #CHF
🔓 pubmed.ncbi.nlm.nih.gov
🔓 pubmed.ncbi.nlm.nih.gov
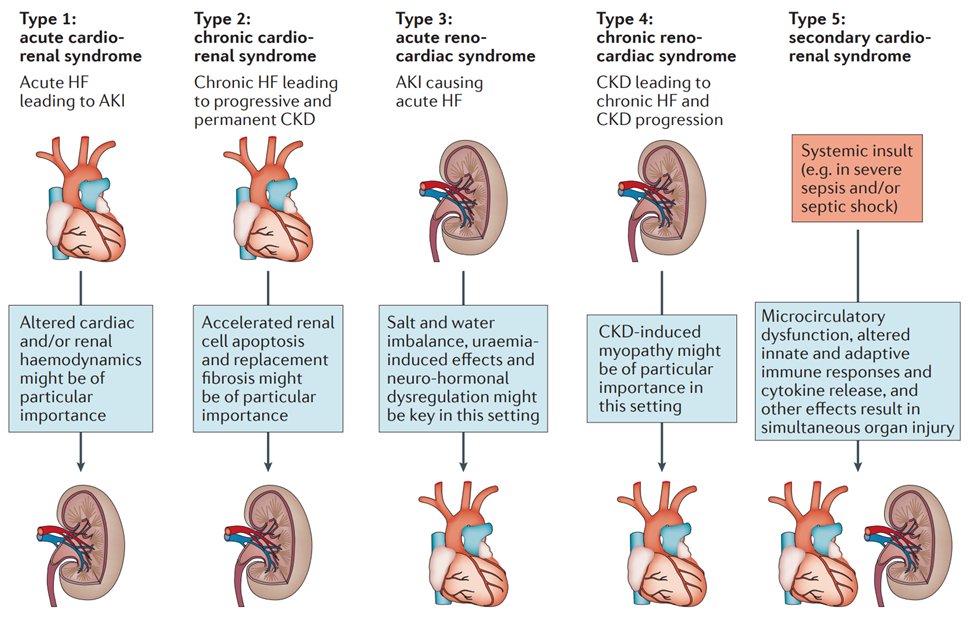
9a) Almost 2 decades ago, @croncoIRRIV et al suggested that at least five conceptual #Cardiorenal subtypes may exist #Nephpearls
🔓 pubmed.ncbi.nlm.nih.gov
pubmed.ncbi.nlm.nih.gov
🔓 pubmed.ncbi.nlm.nih.gov
pubmed.ncbi.nlm.nih.gov
pubmed.ncbi.nlm.nih.gov/19007588/
Cardiorenal syndrome - PubMed
The term cardiorenal syndrome (CRS) increasingly has been used without a consistent or well-accepted...

pubmed.ncbi.nlm.nih.gov/27573728/
Heart failure and kidney dysfunction: epidemiology, mechanisms and management - PubMed
Heart failure (HF) is a major health-care problem and the prognosis of affected patients is poor. HF...
9b) Although this classification has been of great value for awareness for researchers & clinicians, as well as the ID of pts, it is based largely on expert opinion. Data to support the distinction based on pathophys, tx, & prognosis are limited.
🔓 pubmed.ncbi.nlm.nih.gov
🔓 pubmed.ncbi.nlm.nih.gov
9c) In fact, one could even argue that there is only scarce evidence to classify the #cardiorenal syndrome as a true distinct entity as it could merely be regarded as a physiological (and passive) response of the kidney to a failing heart.
🔓 pubmed.ncbi.nlm.nih.gov
🔓 pubmed.ncbi.nlm.nih.gov
10a) Since the early 2000s, the definition of #cardiorenal syndrome #CRS has evolved
pubmed.ncbi.nlm.nih.gov
pubmed.ncbi.nlm.nih.gov
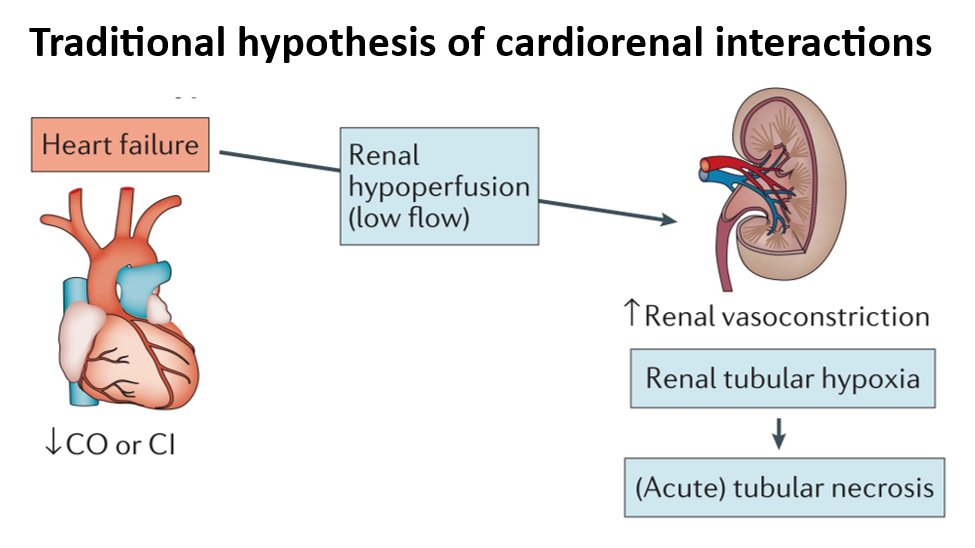
10b) Traditional hypothesis of how renal dysfunction develops in #HF is that it results from heart failure-induced hypoperfusion of the kidneys (low flow), which was thought to ⬆️renal vasoconstriction ➡️renal tubular hypoxia & tubular necrosis
pubmed.ncbi.nlm.nih.gov
pubmed.ncbi.nlm.nih.gov
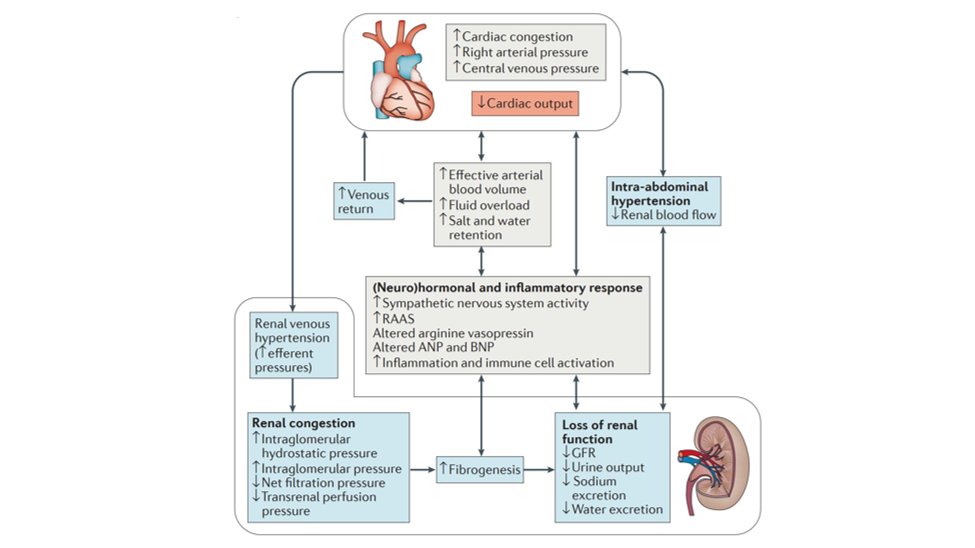
10c) #Kidney dysfunction in heart failure is now also thought to develop as a result of reduced cardiac output, which results in increased cardiac congestion, increased right atrial pressure, and increased central venous pressure
10d) The changes to kidney function as a consequence of ⬇️ cardiac output result in the development of renal venous hypertension, renal venous congestion, ⬆️ renal fibrogenesis, and eventually the loss of kidney function
pubmed.ncbi.nlm.nih.gov
pubmed.ncbi.nlm.nih.gov
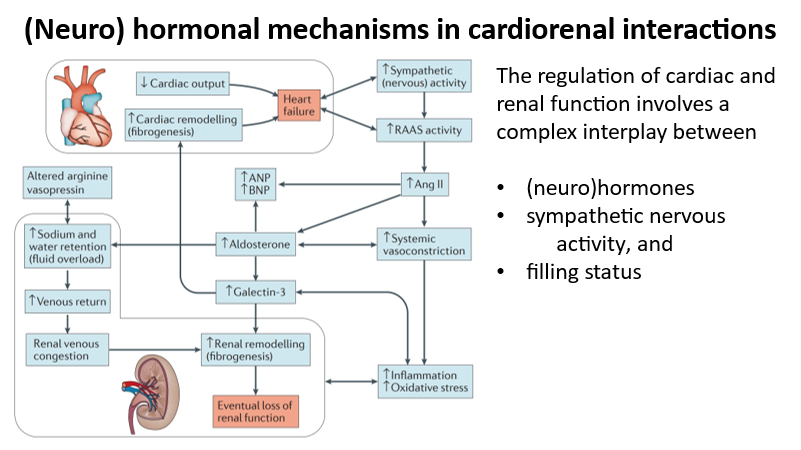
11a) The regulation of cardiac and kidney function involves a complex interplay between (neuro)hormones, sympathetic nervous activity, and filling status
pubmed.ncbi.nlm.nih.gov
pubmed.ncbi.nlm.nih.gov
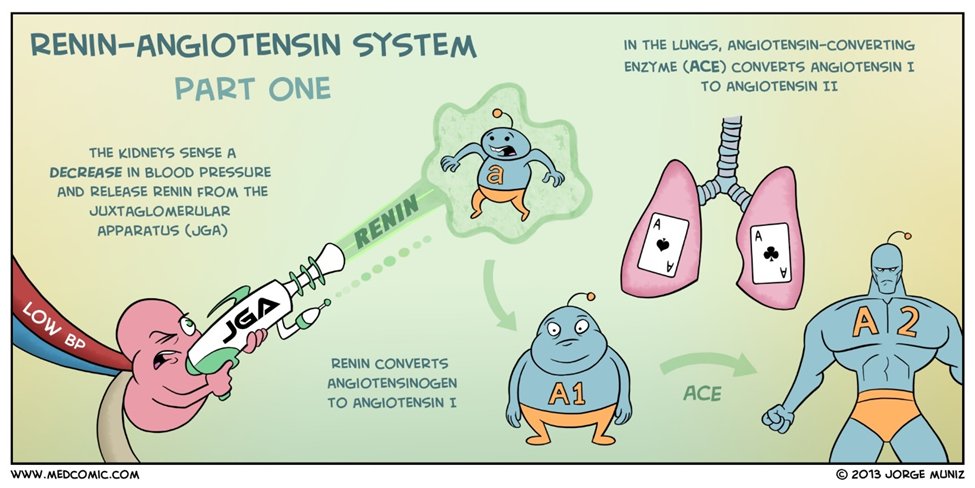
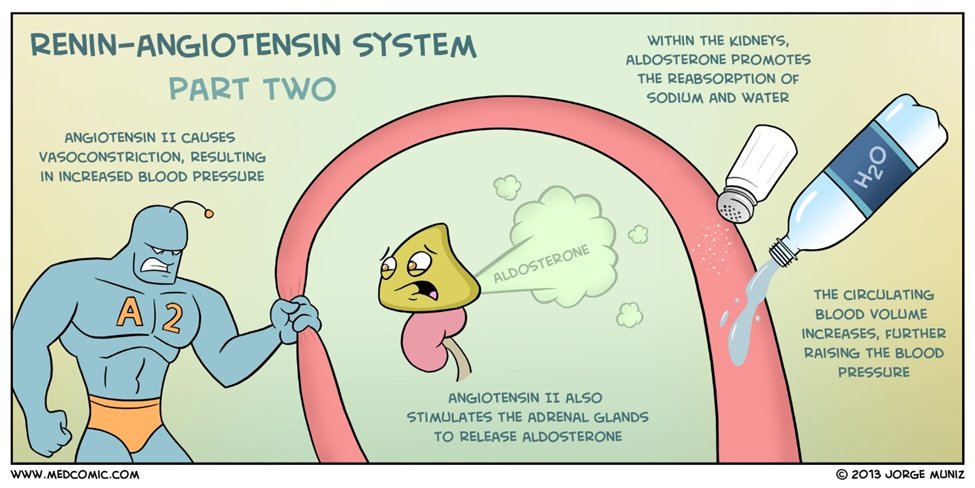
11b) Key mediators that promote a (neuro)hormonal imbalance include increased activation of the renin–angiotensin–aldosterone system (#RAAS), which results in increases in #angiotensin II (ang II) and #aldosterone and a reduction in renal salt and water excretion
11c) Increased sympathetic nervous activity can further enhance #RAAS-mediated fluid overload and increase systemic vasoconstriction
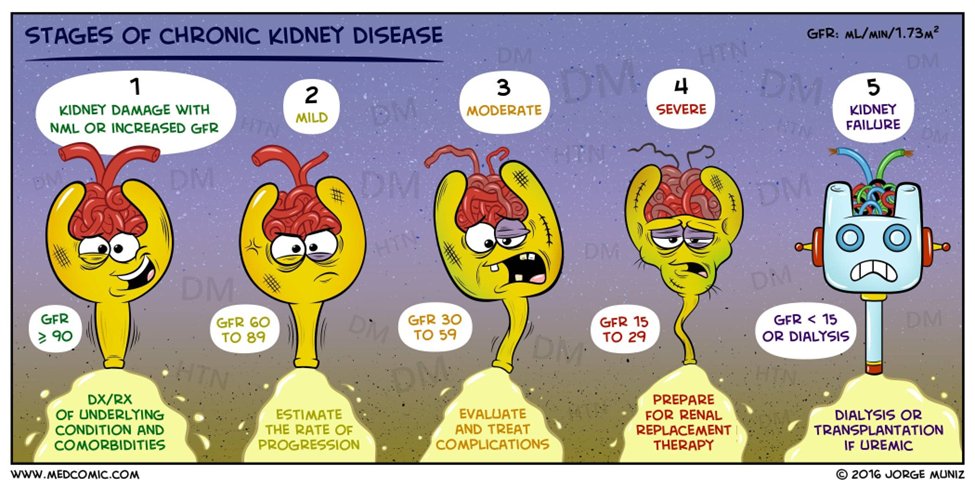
#VisualArt by @medcomic
#VisualArt by @medcomic
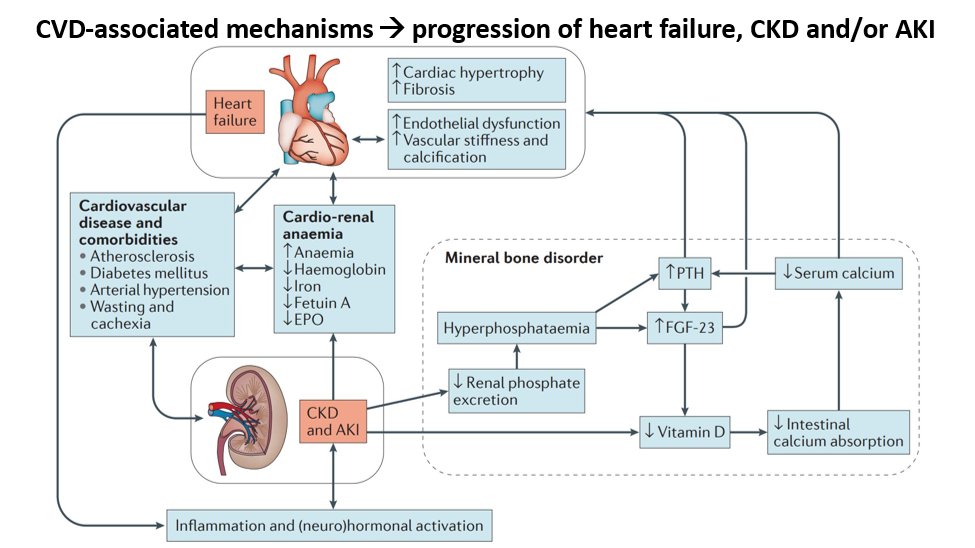
12a) #Cardiovascular disease-associated mechanisms leading to the progression of #heart failure, chronic kidney disease (#CKD), and/or acute kidney injury (#AKI) include systemic #atherosclerosis, #DM, #htn, and wasting & cachexia.
pubmed.ncbi.nlm.nih.gov
pubmed.ncbi.nlm.nih.gov
12c) . . . and/or bone and mineral disorder, which can be triggered by conditions associated with #CKD and #AKI, such as #hyperphosphatemia
🔓 pubmed.ncbi.nlm.nih.gov
🔓 pubmed.ncbi.nlm.nih.gov
12e) In combination with systemic inflammatory and/or (neuro)hormonal mechanisms the increase in #PTH and FGF-23 can augment chronic or acute kidney injury and/or cardiac disease via remodeling and/or #fibrogenesis & through the consecutive loss of organ function
13) Going back to our canary in the coal mine metaphor, what can we use as our canary to warn us of danger ahead?
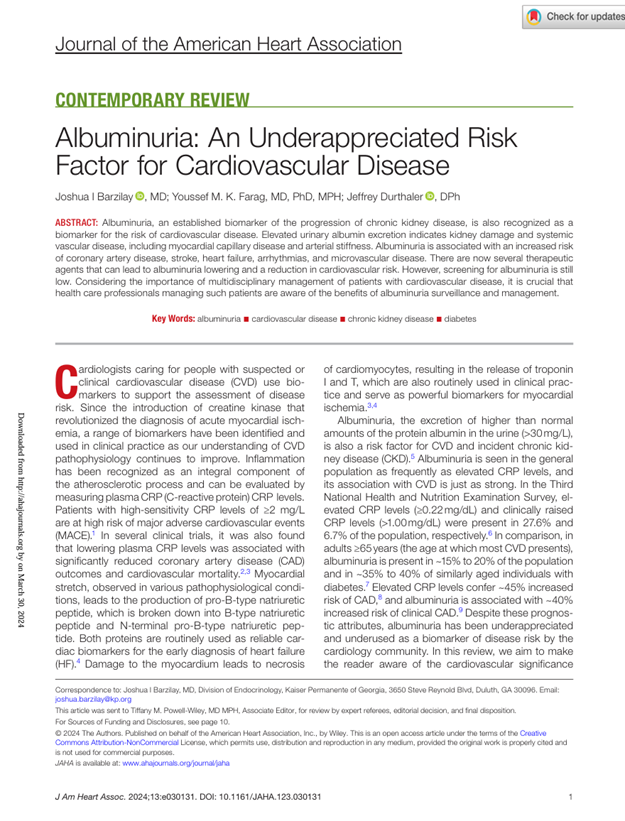
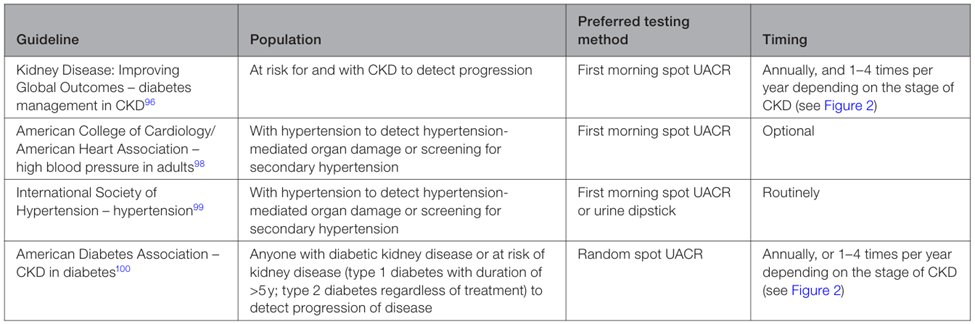
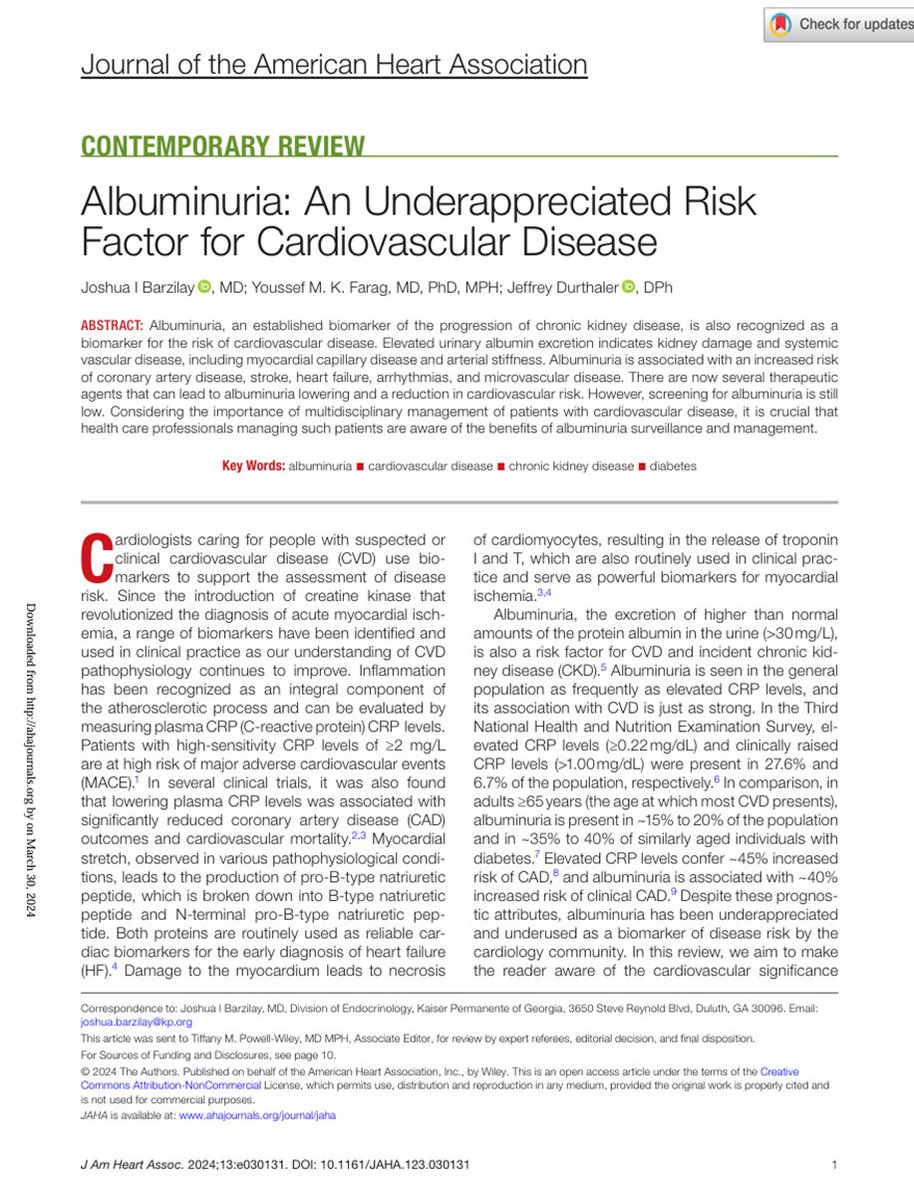
This table shows the associations of #albuminuria with #cardiovascular disease
#Nephpearls #Cardiorenal
🔓 pubmed.ncbi.nlm.nih.gov
This table shows the associations of #albuminuria with #cardiovascular disease
#Nephpearls #Cardiorenal
🔓 pubmed.ncbi.nlm.nih.gov
14a) #Albuminuria refers to abnormal loss of albumin in the urine (urine #ACR ≥30 mg/g or ≥3 mg/mmol).
Albumin is one type of plasma protein found in the urine in normal subjects and in larger quantity in people with kidney disease
🔓 kdigo.org
Albumin is one type of plasma protein found in the urine in normal subjects and in larger quantity in people with kidney disease
🔓 kdigo.org
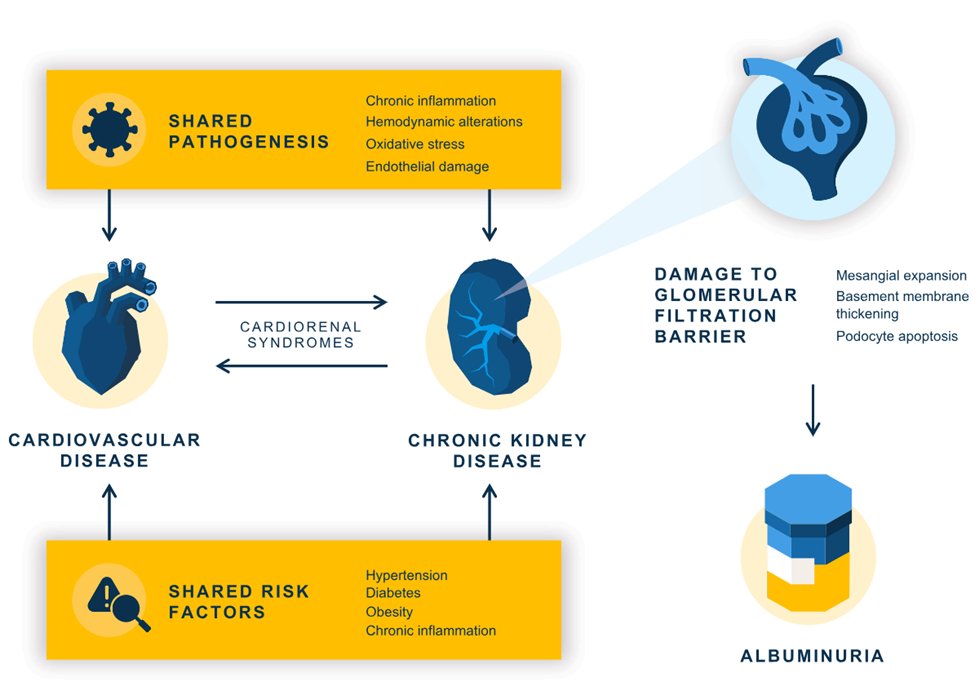
14b) The physiologic role of albumin is to maintain plasma oncotic pressure & to transport various endogenous & exogenous ligands through the bloodstream to target cells
14c) In healthy individuals, the endothelial layer of the glomerulus serves as a barrier that minimizes albumin movement from the blood into the urine
14d) Albuminuria involves structural damage in the glomerulus, which is associated with an increased risk for undesirable cardiovascular and kidney outcomes
🔓 pubmed.ncbi.nlm.nih.gov
🔓 pubmed.ncbi.nlm.nih.gov
15a) #Cardiovascular and kidney disease share many risk factors and pathological processes that can lead to #albuminuria. Injury to the glomerulus resulting in albuminuria is seen in #CVD . . .
15b) . . . because of the shared pathological processes with #CKD and because of compensatory mechanisms in chronic #cardiovascular disease #Nephpearls #Cardiorenal
🔓 pubmed.ncbi.nlm.nih.gov
🔓 pubmed.ncbi.nlm.nih.gov
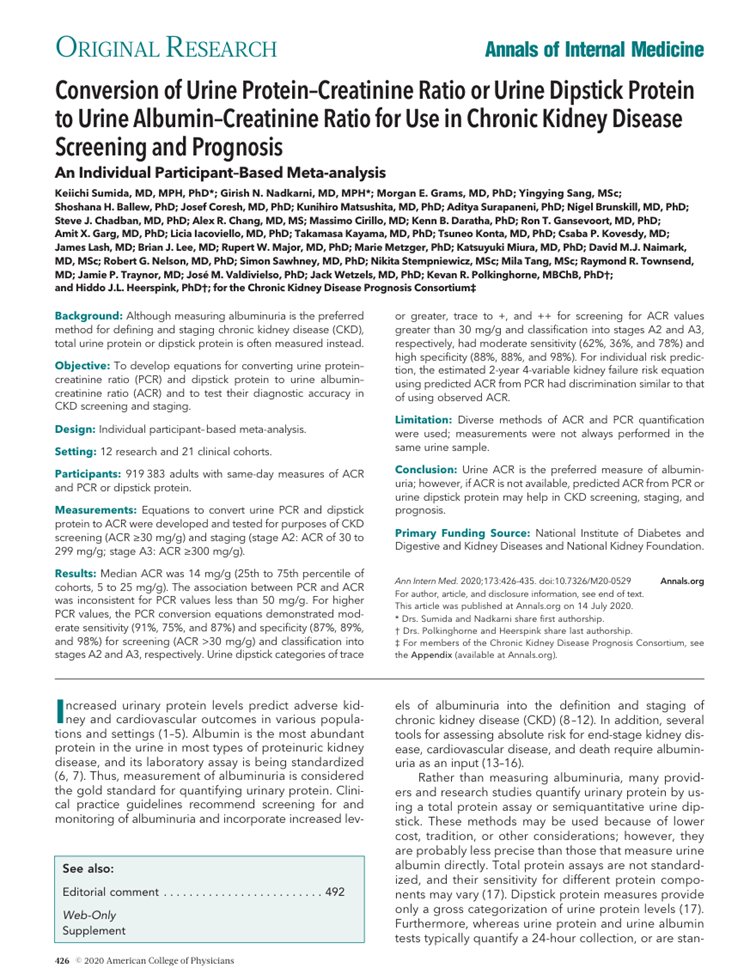
16a) What do we call it?? #Albuminuria or #Proteinuria?
16b) In the @goKDIGO 2012 Clinical Practice Guideline for the Evaluation and Management of #CKD, clinical terminology was changed to focus on #albuminuria rather than #proteinuria as albumin is the principal component of urinary protein in most kidney diseases
16d) In addition, assays to measure #albumin are more precise & sensitive than those used to measure urine protein
🔓 pubmed.ncbi.nlm.nih.gov
#VisualAbstract by @AnnaGaddy
🔓 pubmed.ncbi.nlm.nih.gov
#VisualAbstract by @AnnaGaddy
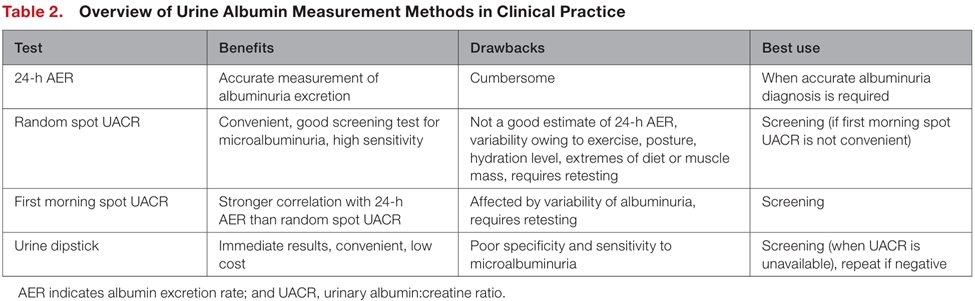
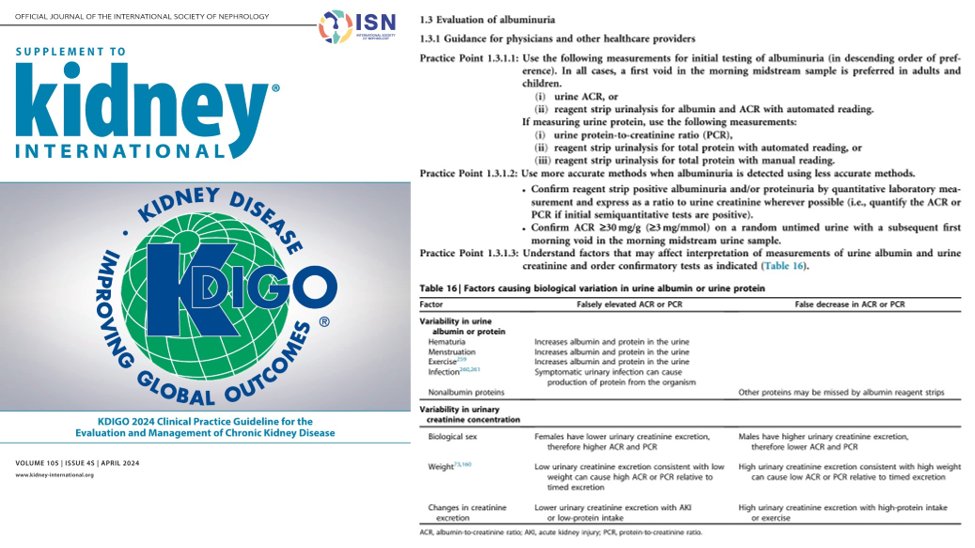
17a) Recognizing the limitations of testing & variable availability of resources, the @goKDIGO provides some guidance regarding following measurements for initial testing for #albuminuria and/ or #proteinuria
#Nephpearls #Cardiorenal
🔓 kdigo.org
#Nephpearls #Cardiorenal
🔓 kdigo.org
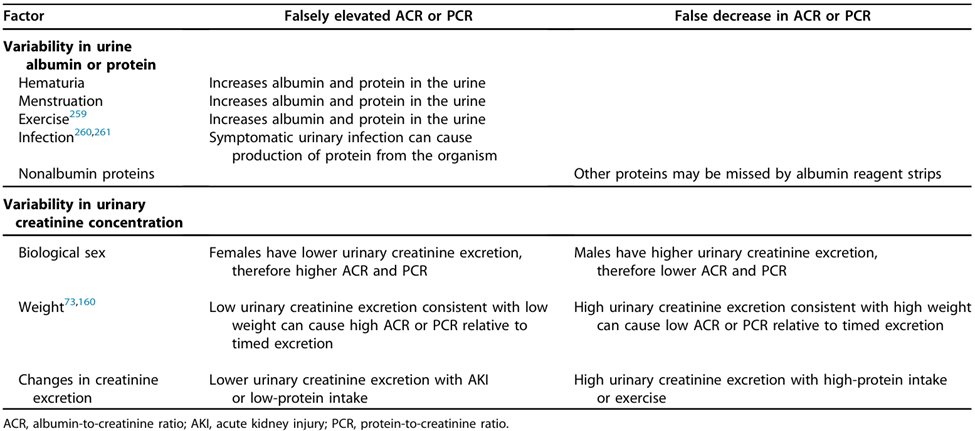
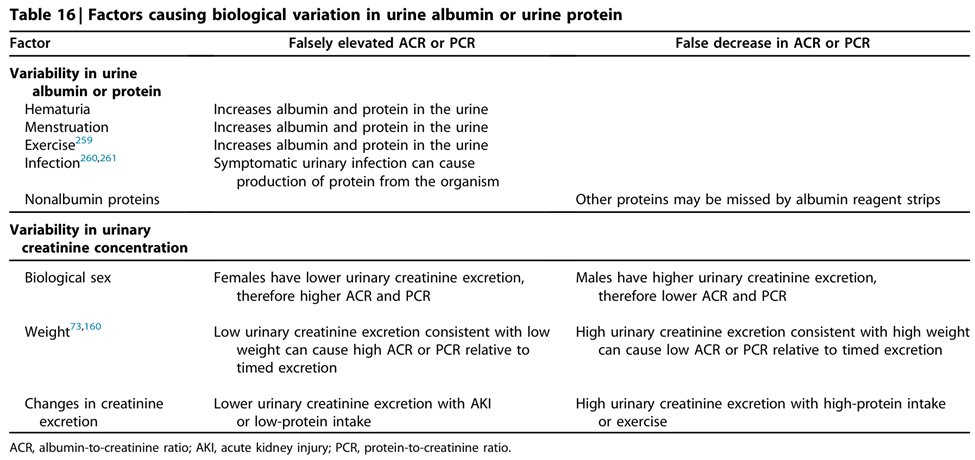
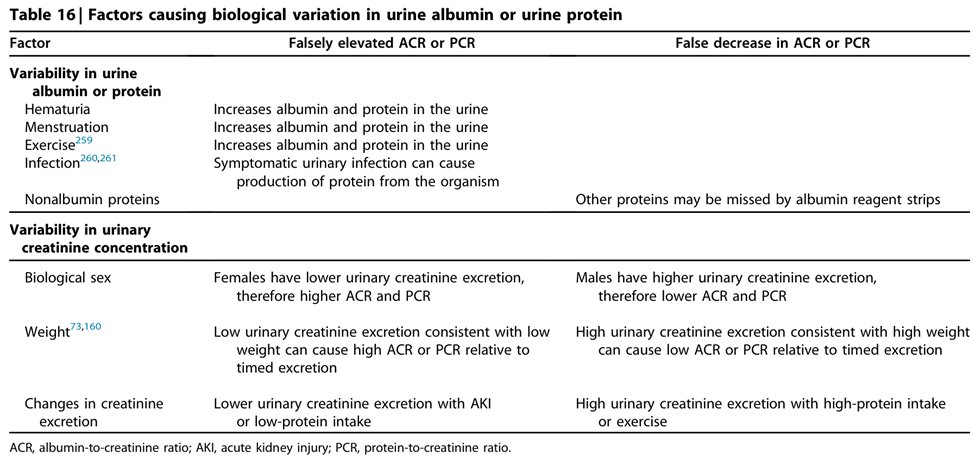
17b) It is also important to recognize that there are factors causing biological variation in urine albumin or urine protein, thereby significantly affecting the interpretation of these tests in certain circumstances
#Nephpearls #Cardiorenal
🔓 kdigo.org
#Nephpearls #Cardiorenal
🔓 kdigo.org
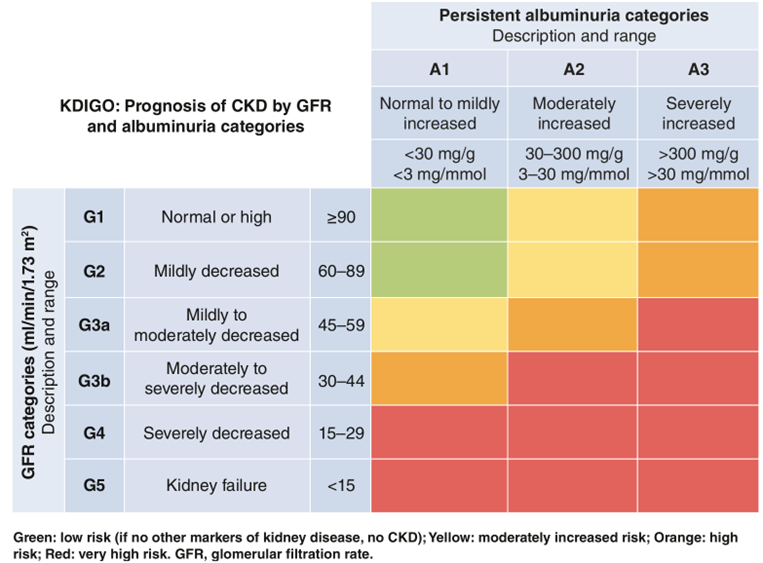
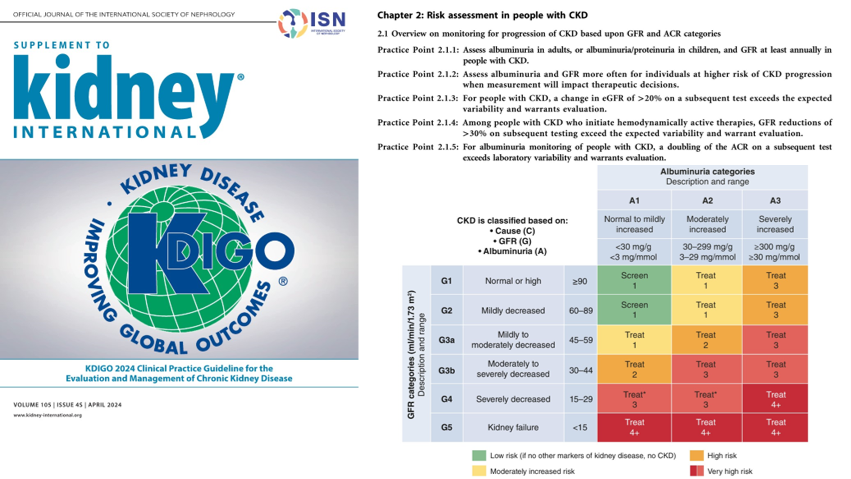
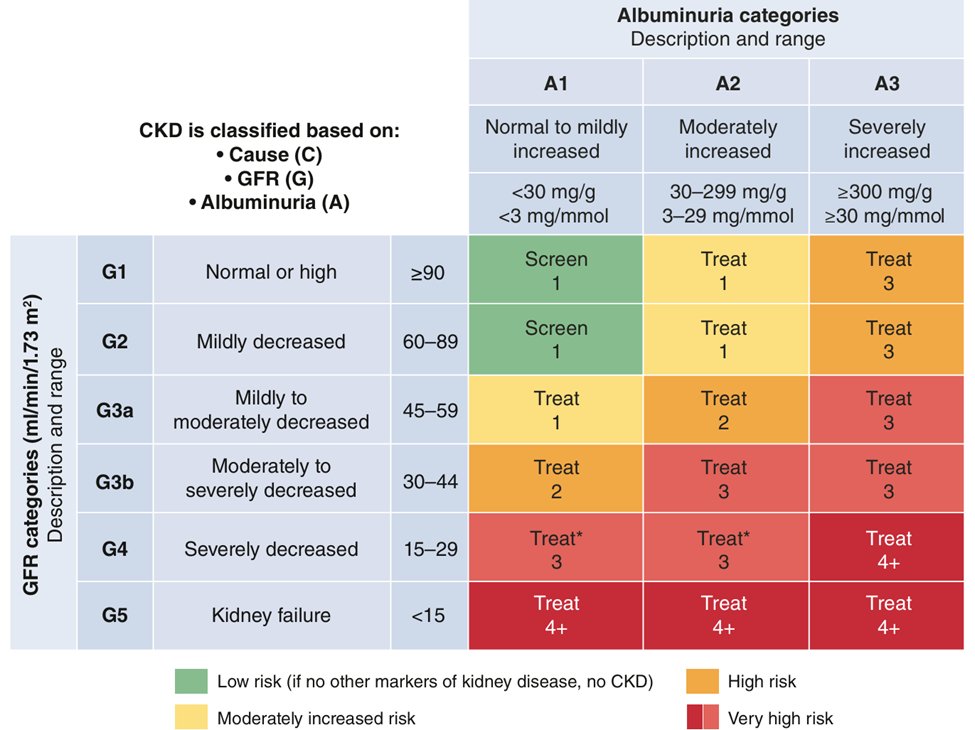
18a) #Albuminuria is classified into 1 of 3 categories, A1 to A3, depending on the severity
#Nephpearls #Cardiorenal
🔓 kdigo.org
#Nephpearls #Cardiorenal
🔓 kdigo.org
18b) There are several methods to detect albuminuria in daily clinical practice
Studies examining the diagnostic accuracy of tests to quantify urine #albumin and other proteins usually compare tests with laboratory quantification from 24-hour urine collections
Studies examining the diagnostic accuracy of tests to quantify urine #albumin and other proteins usually compare tests with laboratory quantification from 24-hour urine collections
18c) It is generally recognized that a 24-hour sample is the definitive means of demonstrating the presence of albuminuria
However, this test is cumbersome and not convenient for routine clinical practice
🔓 pubmed.ncbi.nlm.nih.gov
However, this test is cumbersome and not convenient for routine clinical practice
🔓 pubmed.ncbi.nlm.nih.gov
18d) Because #creatinine excretion in the urine is fairly constant throughout the 24 hour period, the measurement of ACR (or PCR) allows correction for variations in urinary concentration
ACR is a suitable alternative to timed measurement of urine albumin loss
ACR is a suitable alternative to timed measurement of urine albumin loss
18e) PCR on random or early morning untimed samples shows good diagnostic performance and correlation with 24-hour collection
18f) The numeric equivalence of #ACR in mg/g (mg/mmol) to approximately g/d is based on the simple assumption that creatinine excretion rate (CER) approximates 1 gram/d (10 mmol/d)
18g) Measurement of urinary #albumin is recommended because it is relatively standardized and because it is the single most important protein lost in the urine in most CKDs
18h) Use of urinary albumin measurement as the preferred test for proteinuria detection will improve the sensitivity, quality, and consistency of approach to the early detection and management of kidney disease
18i) Because the amount of creatinine excreted into the urine varies, the ratio of albumin to creatinine is only an approximation of 24-hour ACR
🔓 kdigo.org
🔓 kdigo.org
19a) Elevated levels of urine albumin are one of the earliest signs of #CKD and damage of the kidney microvasculature
19b) It follows that screening for ⬆️urine #albumin & managing pts early on have the potential to lower the risk of end-stage kidney failure (need for #dialysis or #transplantation) and the risk of concomitant #cardiovascular complications including #ischemia, #arrhythmia, & #HF
19c) Several guidelines recommend screening for #albuminuria @goKDIGO @ACCinTouch @American_Heart @ISHBP @AmDiabetesAssn #Nephpearls #Cardiorenal
🔓 pubmed.ncbi.nlm.nih.gov
🔓 pubmed.ncbi.nlm.nih.gov
19d) This is especially so today, given the availability of medications that lower #albuminuria levels and provide #cardiorenal protection
🔓 pubmed.ncbi.nlm.nih.gov
🔓 pubmed.ncbi.nlm.nih.gov
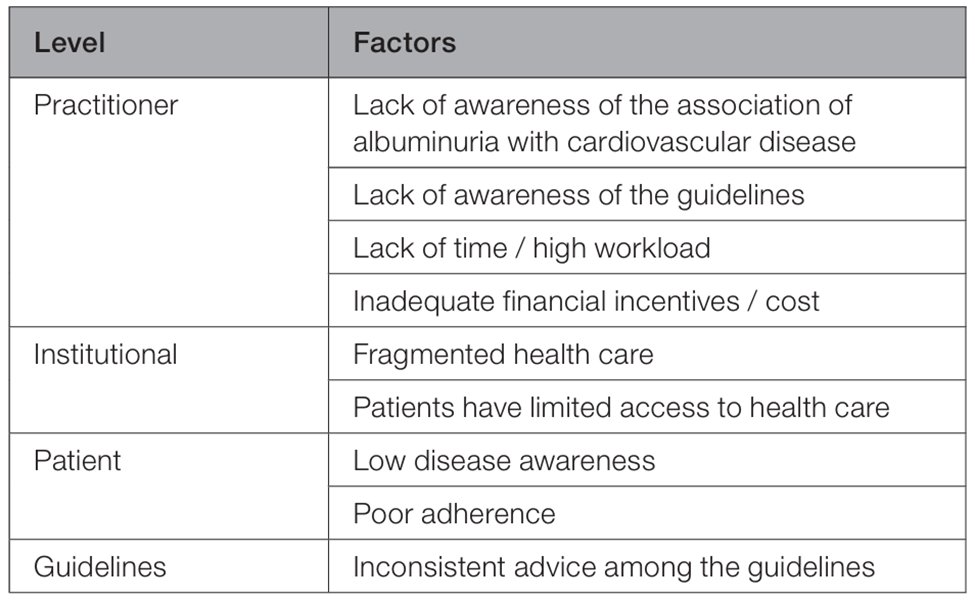
20) Despite this however, there are factors that have been identified that contribute to low albuminuria testing rates
🔓 pubmed.ncbi.nlm.nih.gov
🔓 pubmed.ncbi.nlm.nih.gov
21) In this connection, this is one of the important topics in the Clinical Practice Guideline for the Evaluation and Management of #CKD that was recently published by @goKDIGO
#VisualArt by @medcomic
🔓 kdigo.org
#VisualArt by @medcomic
🔓 kdigo.org
22a) There is significant emphasis on the importance of detecting CKD, and considerations for the optimal methods for staging of CKD, and how to establish chronicity and etiology
🔓 kdigo.org
🔓 kdigo.org
22c) Early detection of any chronic disease, including #CKD, provides greater opportunities to reduce morbidity as treatments can be initiated earlier in the disease course
22d) Because treatments for CKD provide benefits in reducing risk for both CVD and CKD progression, strategies that promote early detection of CKD should improve kidney and non–kidney related outcomes
🔓 kdigo.org
🔓 kdigo.org
23a) Practice Point 1.1.1.2 from @goKDIGO: Following incidental detection of elevated urinary albumin-to-creatinine ratio (#ACR), #hematuria, or low estimated GFR (#eGFR), repeat tests to confirm presence of CKD
🔓 kdigo.org
🔓 kdigo.org
23b) Evaluation of #albuminuria
Risk Assessment in people with CKD
Practice Point 2.1.1 from @goKDIGO: Assess albuminuria in adults, or albuminuria/ proteinuria in children, and GFR at least annually in people with CKD
Risk Assessment in people with CKD
Practice Point 2.1.1 from @goKDIGO: Assess albuminuria in adults, or albuminuria/ proteinuria in children, and GFR at least annually in people with CKD
23c) Monitoring #CKD through the surveillance of #albuminuria and #GFR serves to update staging for prognosis, identify timing of intervention strategies, and assess the effectiveness of specific treatments
24a) Practice Point 2.1.2 from @goKDIGO: Assess #albuminuria and #GFR more often for individuals at higher risk of #CKD progression when measurement will impact therapeutic decisions
24b) More frequent monitoring may be indicated in people with changing clinical status, intercurrent events, and after therapeutic interventions to assess response and adherence and ensure safety
24c In addition, progression risk may vary by the etiology of CKD within a specific stage based on GFR and albuminuria or proteinuria
🔓 kdigo.org
🔓 kdigo.org
25a) Practice Point 2.1.5 from @goKDIGO: For #albuminuria monitoring of people with #CKD, a doubling of the #ACR on a subsequent test exceeds laboratory variability and warrants evaluation
25b) Small fluctuations in #albuminuria or #proteinuria levels may not indicate disease progression
Appreciation of factors that impact albuminuria and changes in the measure is also important for healthcare providers
🔓 kdigo.org
Appreciation of factors that impact albuminuria and changes in the measure is also important for healthcare providers
🔓 kdigo.org
26a) Routine surveillance w/ ACR or PCR is warranted in higher risk people w/CKD, as changes in urine #ACR are assoc'd w/ kidney failure
In large population studies, a doubling of ACR within a 2yr duration is assoc'd w/ an ⬆️in risk of progression to kidney failure by 50%–100%
In large population studies, a doubling of ACR within a 2yr duration is assoc'd w/ an ⬆️in risk of progression to kidney failure by 50%–100%
26b) However, changes in albuminuria within an individual have substantial variability, with large fluctuations expected given that the 95% CI around repeat ACR testing is approximately 50%
26c) For this reason, the @goKDIGO Work Group has defined a doubling in albuminuria or more as exceeding the expected variability and warranting evaluation if replicated upon repeat testing
26d) Conversely, reductions of the ACR by up to 50% are also consistent with random fluctuation
🔓 kdigo.org
🔓 kdigo.org
27a) In conclusion:
🔑 Albuminuria is a marker of increased physiological stress and an indicator of the need for intensive medical attention
🔑 Its recognition and treatment could lead to improved medical outcomes and reduced medical costs
🔑 Albuminuria is a marker of increased physiological stress and an indicator of the need for intensive medical attention
🔑 Its recognition and treatment could lead to improved medical outcomes and reduced medical costs
27b)
🔑 It is well established that there is a strong as sociation of albuminuria with several manifestations of CVD and CVD mortality
🔑 Despite this knowledge, rates of albuminuria screening in high-risk patients, such as those with diabetes or hypertension, are low
🔑 It is well established that there is a strong as sociation of albuminuria with several manifestations of CVD and CVD mortality
🔑 Despite this knowledge, rates of albuminuria screening in high-risk patients, such as those with diabetes or hypertension, are low
27c) 🔑 Health care professionals are urged to screen for albuminuria per current guidelines
Improving adherence to recommended albuminuria testing guidelines is likely to provide substantial clinical and economic benefits
Improving adherence to recommended albuminuria testing guidelines is likely to provide substantial clinical and economic benefits
27d)
🔑 Albuminuria diagnosis supports the identification of patients at risk of #CVD and #CKD and presents a crucial early opportunity to intervene with cardiorenal-protective therapy to slow disease progression and improve patient outcomes
🔓 pubmed.ncbi.nlm.nih.gov
🔑 Albuminuria diagnosis supports the identification of patients at risk of #CVD and #CKD and presents a crucial early opportunity to intervene with cardiorenal-protective therapy to slow disease progression and improve patient outcomes
🔓 pubmed.ncbi.nlm.nih.gov
27e) The @goKDIGO Guidelines have provided guidance on who to screen, when to screen, and how to manage albuminuria #Nephpearls #Cardiorenal
🔓 kdigo.org
🔓 kdigo.org
28a) So, what have we learned? Elevated levels of WHAT are one of the earliest signs of CKD and damage of the kidney microvasculature?
A. Urine Albumin
B. Serum Creatinine
C. Urine pH
D. Estimated GFR (calculated by CKD-EPI equation)
A. Urine Albumin
B. Serum Creatinine
C. Urine pH
D. Estimated GFR (calculated by CKD-EPI equation)
28c) Epidemiologic data demonstrate a strong relationship between the quantity of urine albumin with both kidney and CVD risk and observed CVD even at very low levels
28d) The following can “falsely increase” albumin and protein in the urine, EXCEPT
A. Hematuria
B. Menstruation
C. Exercise
D. None of the above
A. Hematuria
B. Menstruation
C. Exercise
D. None of the above
28d) It’s D. All of these can ⬆️albuminuria & proteinuria. Small fluctuations in these levels may not always indicate disease progression
Appreciation of factors that impact albuminuria and changes in the measure are also important to know
🔓 kdigo.org
Appreciation of factors that impact albuminuria and changes in the measure are also important to know
🔓 kdigo.org
29) So you just earned 0.75hr 🆓 CE/#CME. Claim it NOW at ckd-ce.com and FOLLOW US so that you don't miss the next #tweetorial from @edgarvlermamd on Early, Optimal Management of #CKD and #Cardiorenal Disease to Prevent Disease Progression and Improve Outcomes!
جاري تحميل الاقتراحات...