Update on what I'm going to now call long COVID symptoms- as it's been 3.5 months since my infection - so am well past the acute stage now. For those who've been following- I've been struggling with breathlessness, chest pain and brain fog post-COVID 🧵
What I've found really debilitating over the past few months is intermittent breathlessness - which occurs on walking, climbing steps, and sometimes just standing up, or walking around the house. It's often accompanied by palpitations (can feel my heart racing), and chest pain.
The symptoms started ~2 wks or so after my acute infection once I started getting out and about and realised that I was getting breathless just on dropping my daughter to school (a twelve minute walk on a very gentle upward slope).
I hadn't even noticed the slope before- but I notice even the most gentle slopes now. I also noticed difficulty with multi-tasking, concentration & memory during this period, but I didn't focus on it much at first because the breathlessness felt far more debilitating and obvious.
But I noticed that I would miss appointments/essential tasks unless I put in a lot more effort- e.g. setting daily alarms & reminders in my calendar for routine task (e.g. school pick ups). I also had difficulty remembering simple things (whether I'd taken my medication).
I don't think it showed as much at work- but I realised the cost of maintaining concentration at meetings was much higher and high often had cognitive equivalent of post-exertion malaise- being exhausted after a day of meetings even if I'd just been sitting at my desk all day.
I had the privilege of being seen by an amazing GP, and consultant, both of whom are very keyed in with long COVID and took my symptoms seriously. I was evaluated for myocarditis, lung clots, and new-onset asthma.
My echocardiogram (test for heart function), cardiac enzymes (test for heart muscle inflammation) were normal. My ventilation-perfusion scan showed slight abnormalities but nothing specific that suggested large clots (cannot rule out microclots with this).
Lung functions (that look for things like new-onset asthma) were also normal.
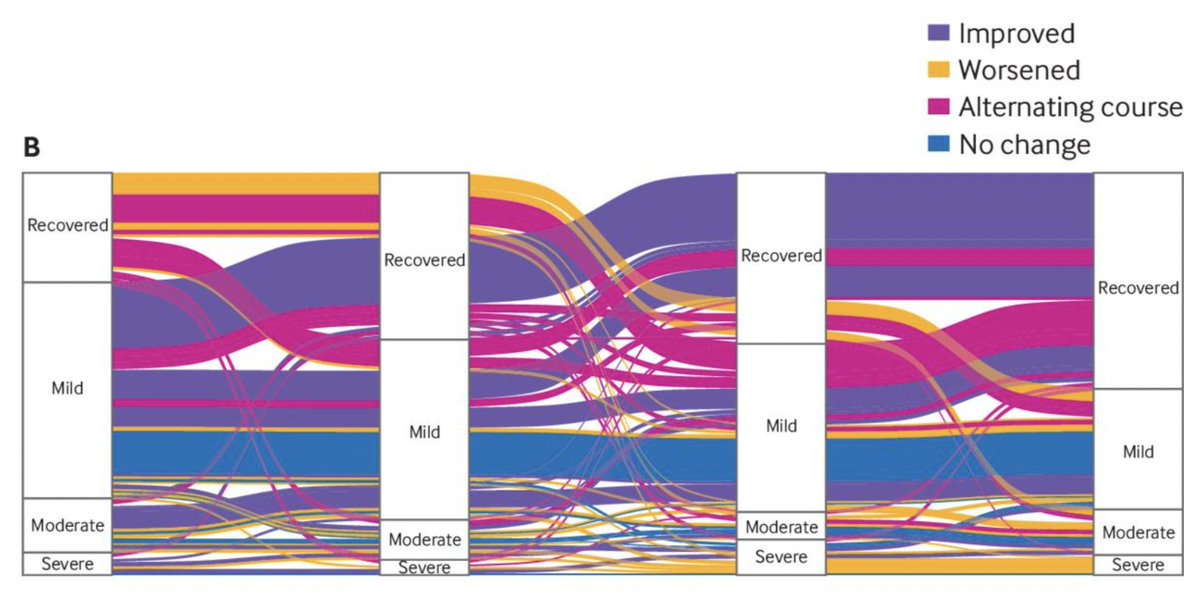
At about 6 weeks or so, I started seeing a regular improvement in symptoms. The improvement wasn't monotonic (as in every day better than the last), but more in the form of fewer bad days than before.
At about 6 weeks or so, I started seeing a regular improvement in symptoms. The improvement wasn't monotonic (as in every day better than the last), but more in the form of fewer bad days than before.
But there was a lot of fluctuation day to day, and it was hard to get a handle on where I'd gotten to in terms of improvement. But slowly I found I was able to walk to school, and on some days even brisk walk without getting breathless. One day I was even able to run with breaks.
My brain fog also improved a lot, and I was able to manage a bigger cognitive load- and do a lot more multi-tasking mentally. It didn't improve to baseline, but in terms of function, I was doing much better, although still at a higher cost of functioning (exhausted afterwards).
Then, oddly about two weeks ago, things took a turn for the worse. I cannot pin-point to anything that necessarily triggered it- but there were days I was breathless just getting out of bed or trying to fix lunch. And needing to stop 2-3 times just walking slowly to school.
The breathlessness and tachycardia has been more frequent- daily for the last week. I don't know what changed this, because I felt I was on a trajectory where things were definitely getting better. I don't know for sure, but I have identified some triggers.
I've noticed that lack of sleep, longer gaps between meals, and heated blankets/hot showers, coffee tend to make it worse. This is what makes me think it's POTS-related - as the breathlessness is accompanied by a high heart rate, but my sats are in the normal range.
I'm not entirely sure what the next steps are- am planning to see a POTS specialist, but wanted to share this - in case there are others who have been hit with very fluctuating symptoms - with promising early improvement followed by worsening - rather than a clear trajectory.
This recent paper from the BMJ shows that a significant proportion of people have a sort of relapsing-remitting course - moving between recovery and symptoms, or different severity categories. So, I guess it isn't unusual.
bmj.com
bmj.com
Still hoping that this will gradually improve over time, although will moderate my expectations better, as the worsening after the early improvement did take me by surprise, and was quite disheartening.
I know I'm one of the lucky ones- I was boostered when I got my infection and was prescribed Paxlovid - all of which reduce risk (and perhaps improve the course?). Unlike many others, I also have the luxury of being able to work from home, and limit my activity.
It does affect me significantly day to day, and has been really debilitating - and I know my symptoms are probably far less severe than many others. I can't imagine having to live with this for years on end - as I know many have been.
Many people made gaslit me & trolled me when I said I was very wary about getting infected because of the risk of long COVID. I have ulcerative colitis, and the few studies done on this and COVID show that the risk of long COVID is between 50-70% for someone with my risk profile
I wasn't believed even by people who were close to me. I knew the probability of long-term symptoms for someone like me was high- with my history of UC, baseline health, being female and immunocompromised. Yet again, there's absolutely no pleasure in having been proved right.
جاري تحميل الاقتراحات...