#AKIConsultSeries
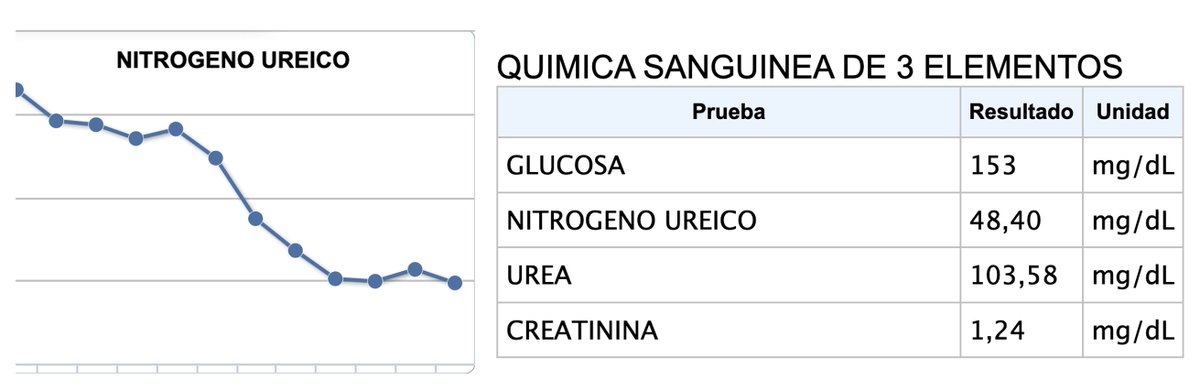
Pt transferred from outside hospital
👴➡️🏥 with altered mental status, 🧠CT ➡️ Intracerebral hemorrhage. Intubated and transfered to our ICU
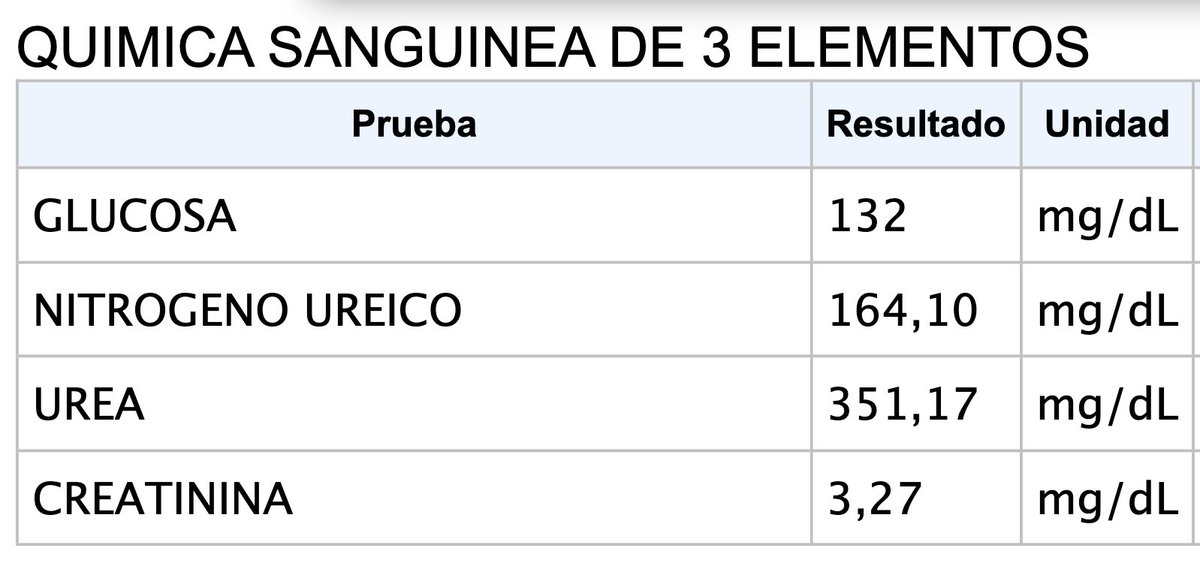
Oliguric, BUN 160 mg/dl and Cr 3.3 mg/dl
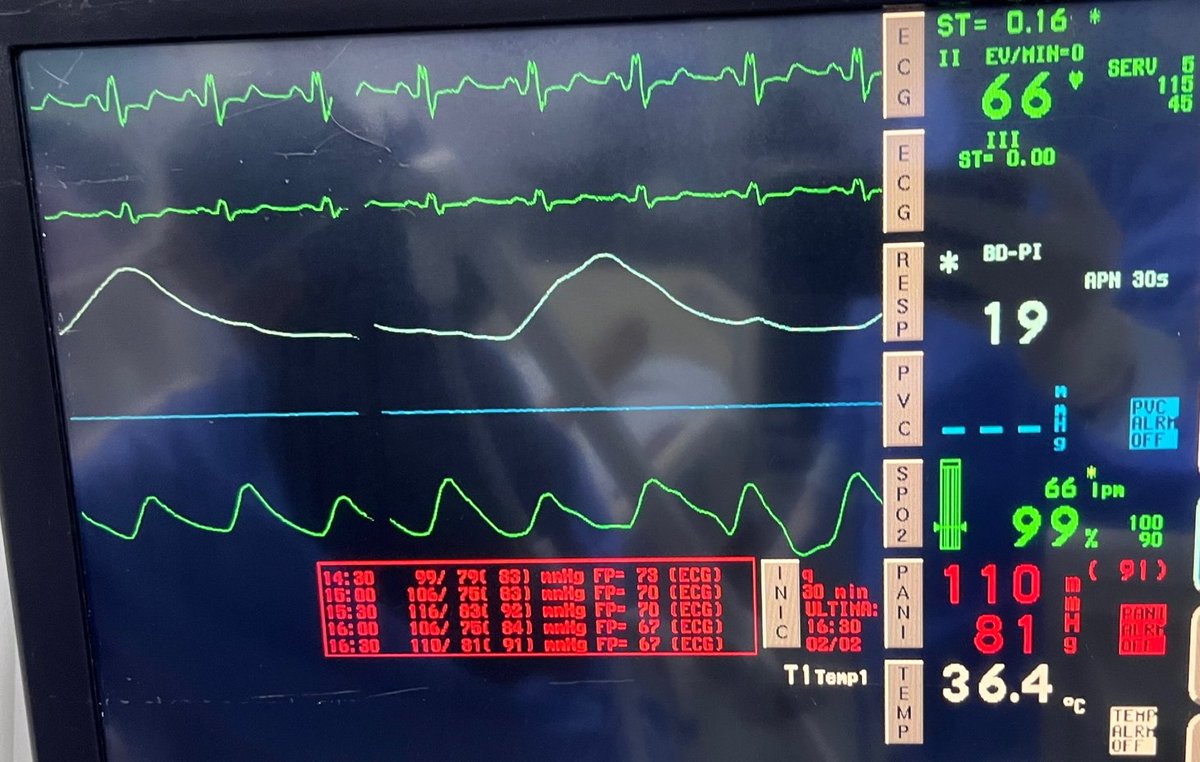
BP 110/81, CRT 2-3 sec, no edema
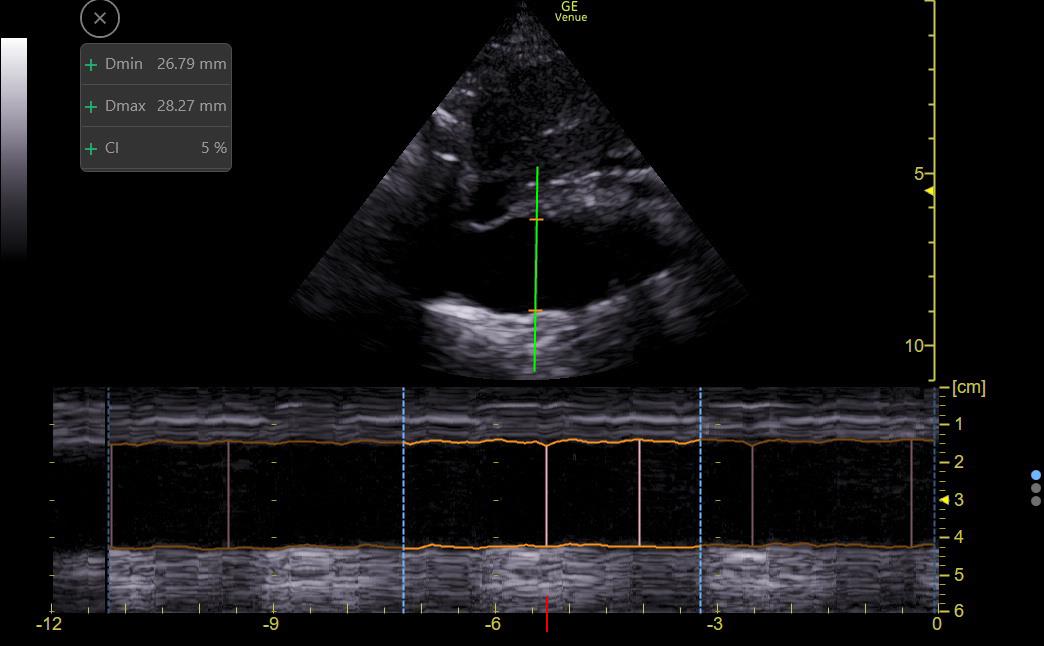
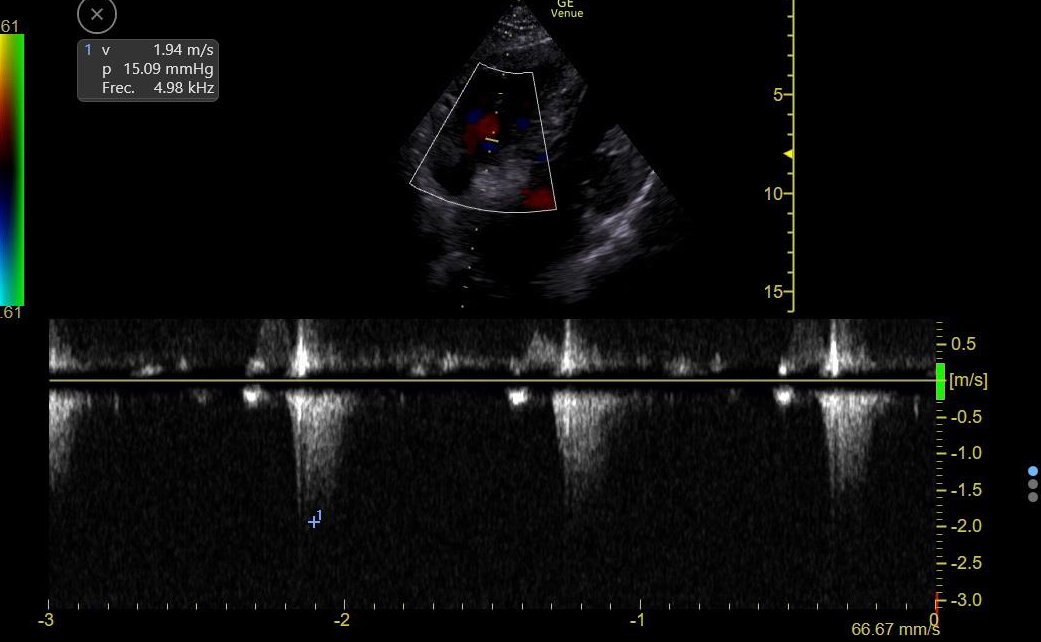
#POCUS ➡️large IVC (2.8 cm)
1/11
Pt transferred from outside hospital
👴➡️🏥 with altered mental status, 🧠CT ➡️ Intracerebral hemorrhage. Intubated and transfered to our ICU
Oliguric, BUN 160 mg/dl and Cr 3.3 mg/dl
BP 110/81, CRT 2-3 sec, no edema
#POCUS ➡️large IVC (2.8 cm)
1/11
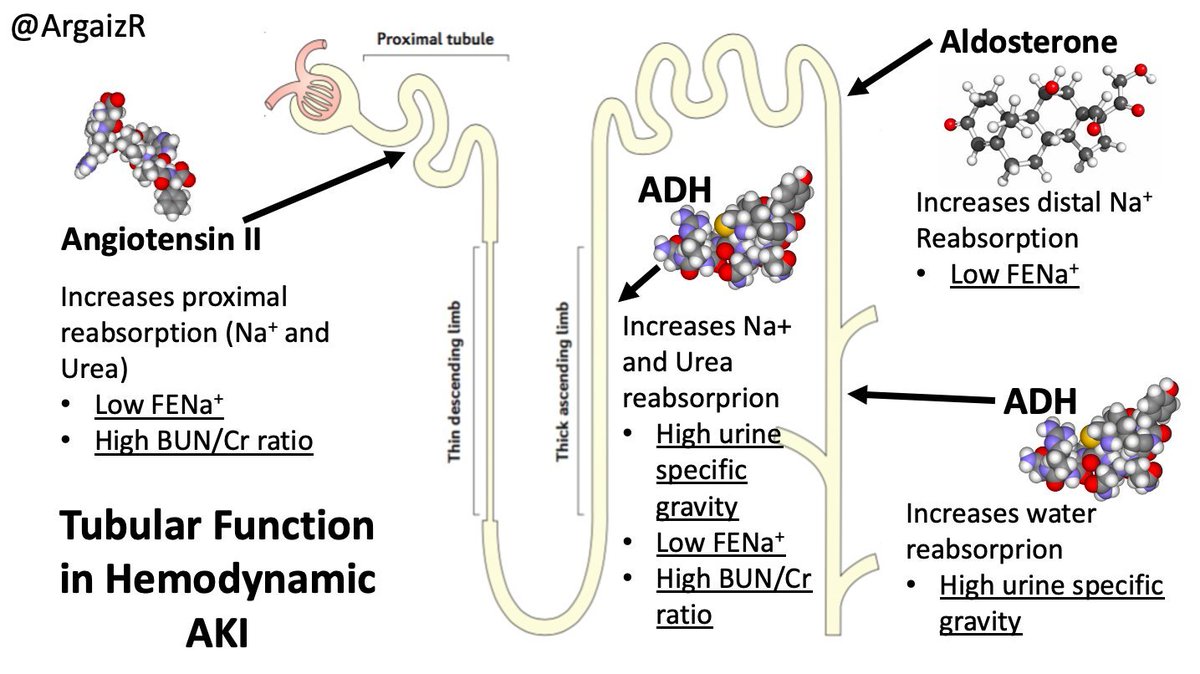
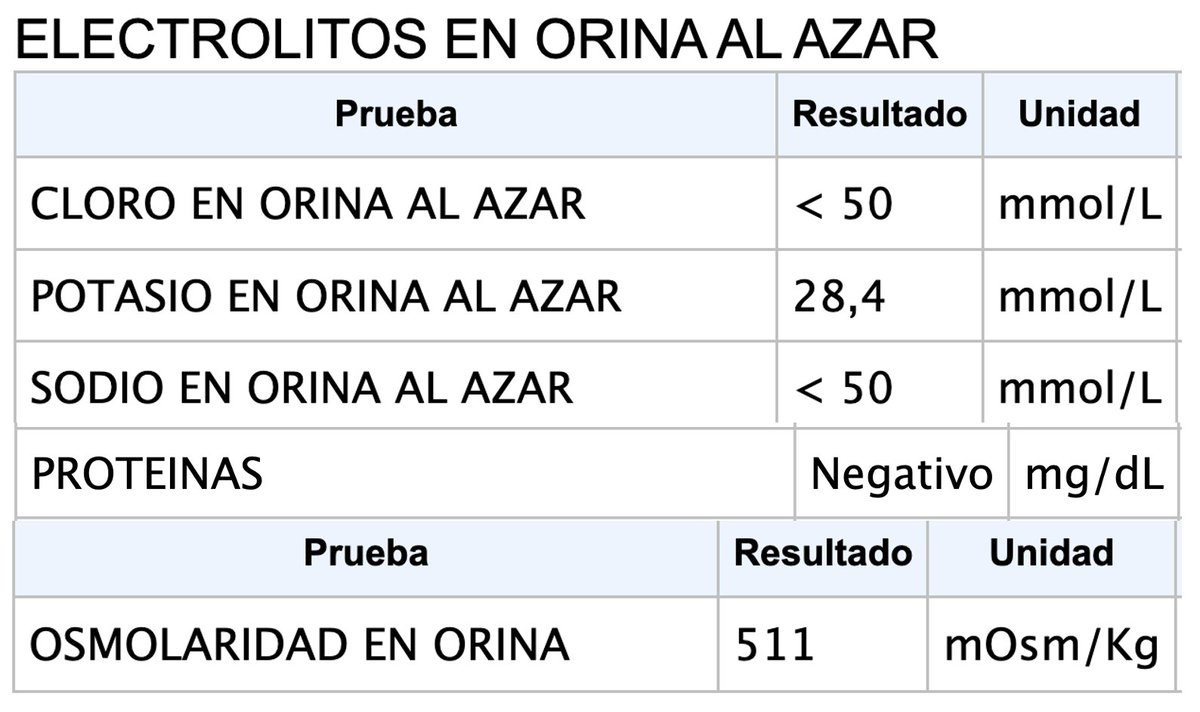
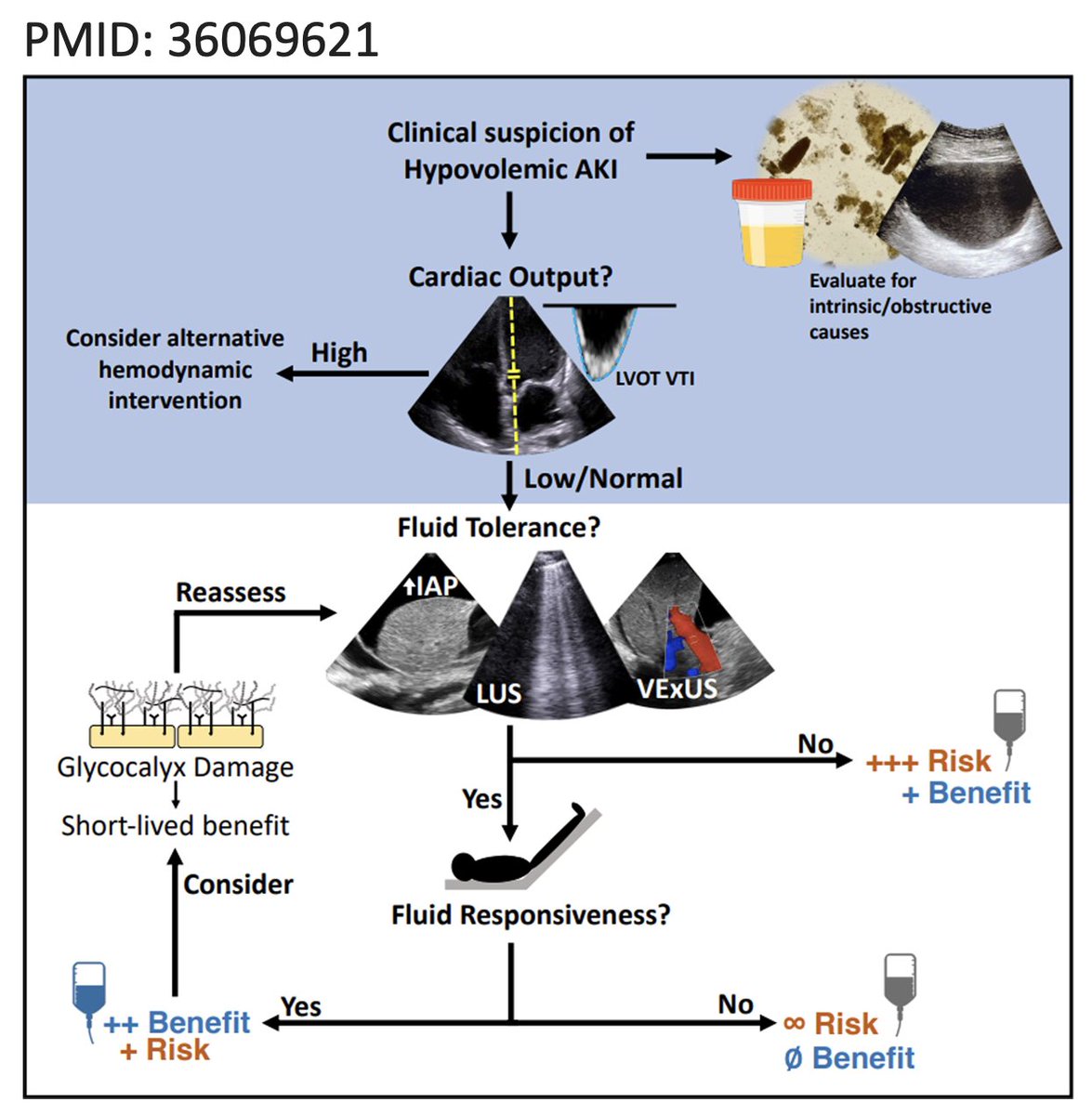
Approach to AKI:
1⃣ The low hanging fruit: Rule out post-renal (#POCUS shows no hydronephrosis and empty bladder)
2⃣Intrinsic vs Hemodynamic
Clues that suggest hemodynamic AKI 👇
This pt had ⬇️ UNa, ⬆️ Uosm, ⬆️ BUN/Cr, no proteinuria and no Granular casts
2/11
1⃣ The low hanging fruit: Rule out post-renal (#POCUS shows no hydronephrosis and empty bladder)
2⃣Intrinsic vs Hemodynamic
Clues that suggest hemodynamic AKI 👇
This pt had ⬇️ UNa, ⬆️ Uosm, ⬆️ BUN/Cr, no proteinuria and no Granular casts
2/11
This all suggests renal tubules are working fine,
There must be a hemodynamic stimulus leading to increased sodium reabsorption and oliguria!
This is Hemodynamic AKI
Is this hypovolemia? Venous Congestion? Distributive? Cardiogenic (low output)?
3/11
There must be a hemodynamic stimulus leading to increased sodium reabsorption and oliguria!
This is Hemodynamic AKI
Is this hypovolemia? Venous Congestion? Distributive? Cardiogenic (low output)?
3/11
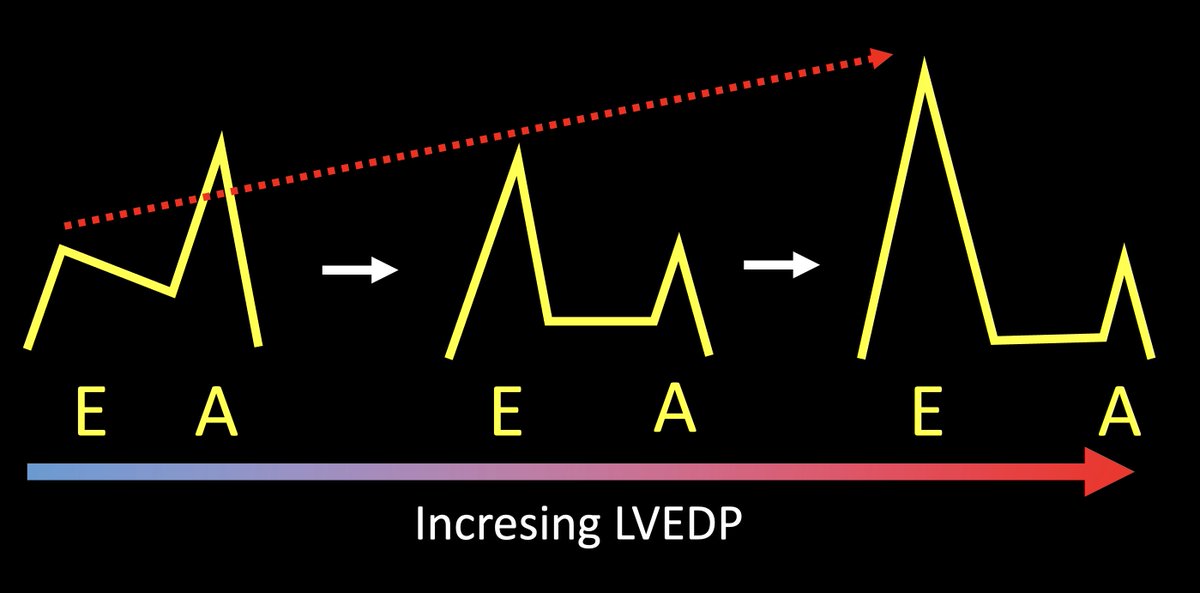
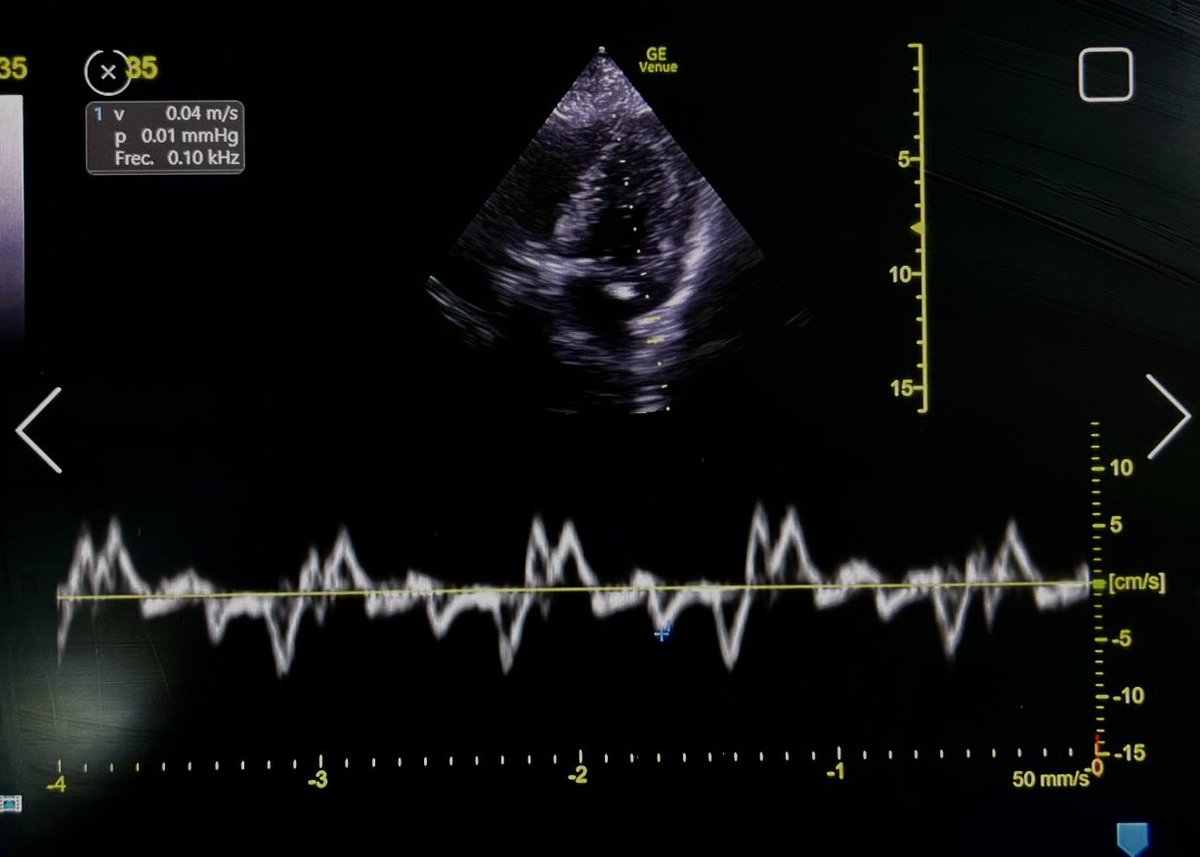
Only subxiphoid window was available:
#EchoFirst:
LV and RV hypertrophy, Moderately ⬇️ LVEF, normal RV function, No tamponade, No RV Failure
These findings strongly argue against:
🔷 Right HF / PAH
🔷 Obstruction (Tamponade, PE)
5/11
#EchoFirst:
LV and RV hypertrophy, Moderately ⬇️ LVEF, normal RV function, No tamponade, No RV Failure
These findings strongly argue against:
🔷 Right HF / PAH
🔷 Obstruction (Tamponade, PE)
5/11
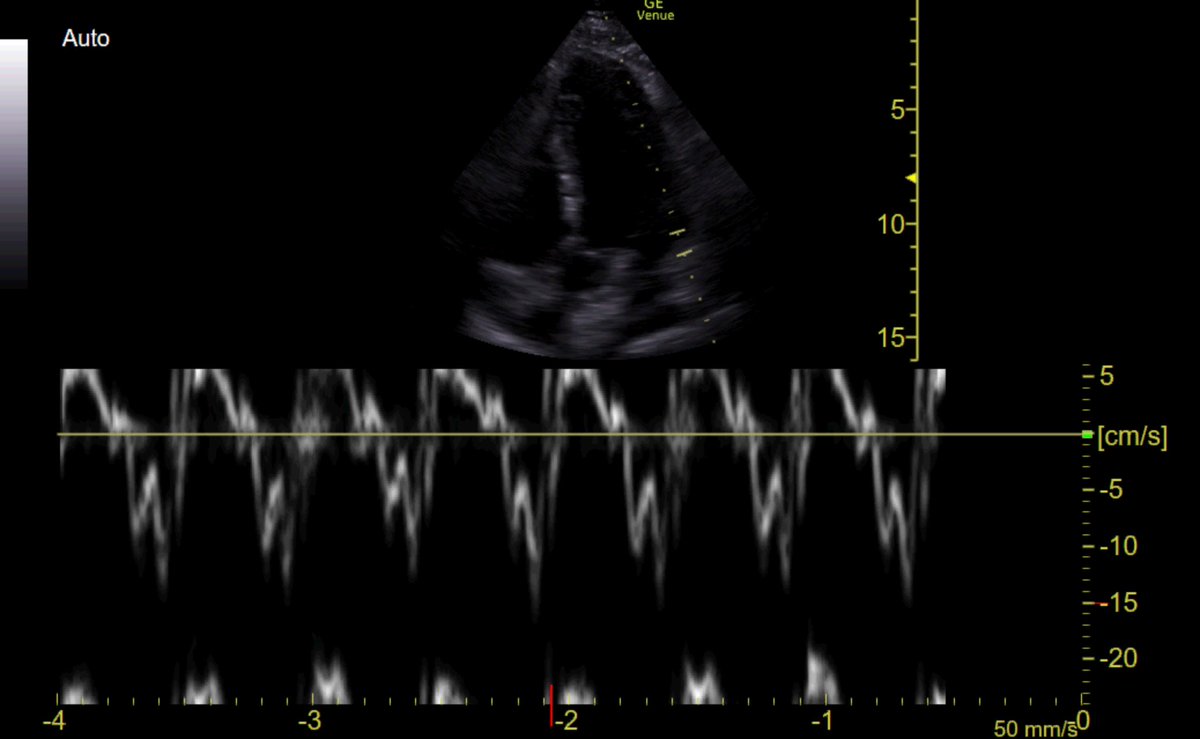
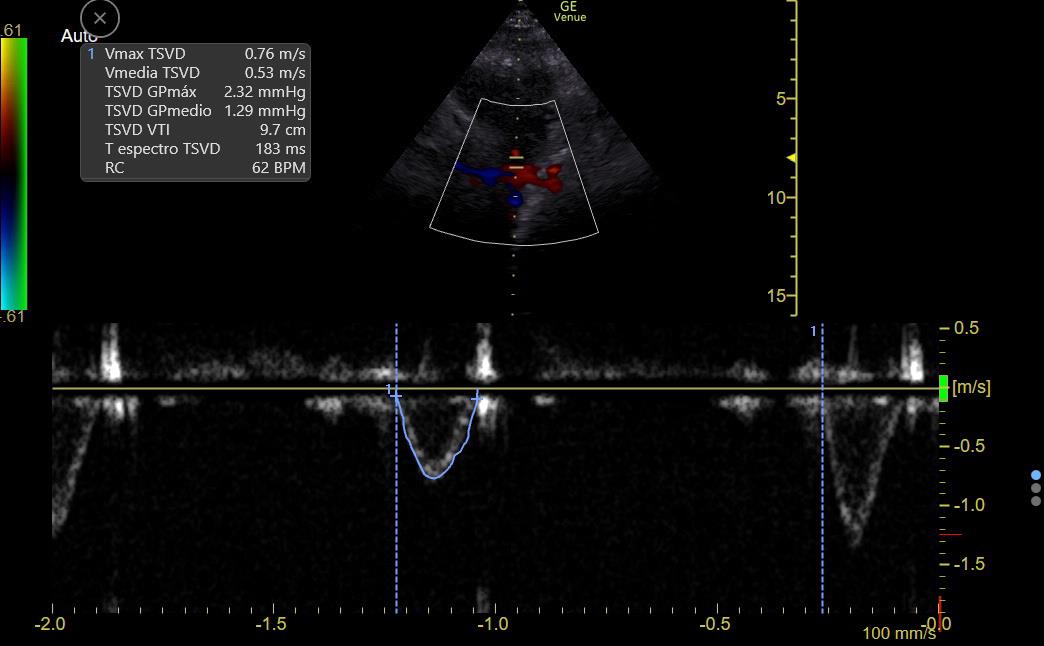
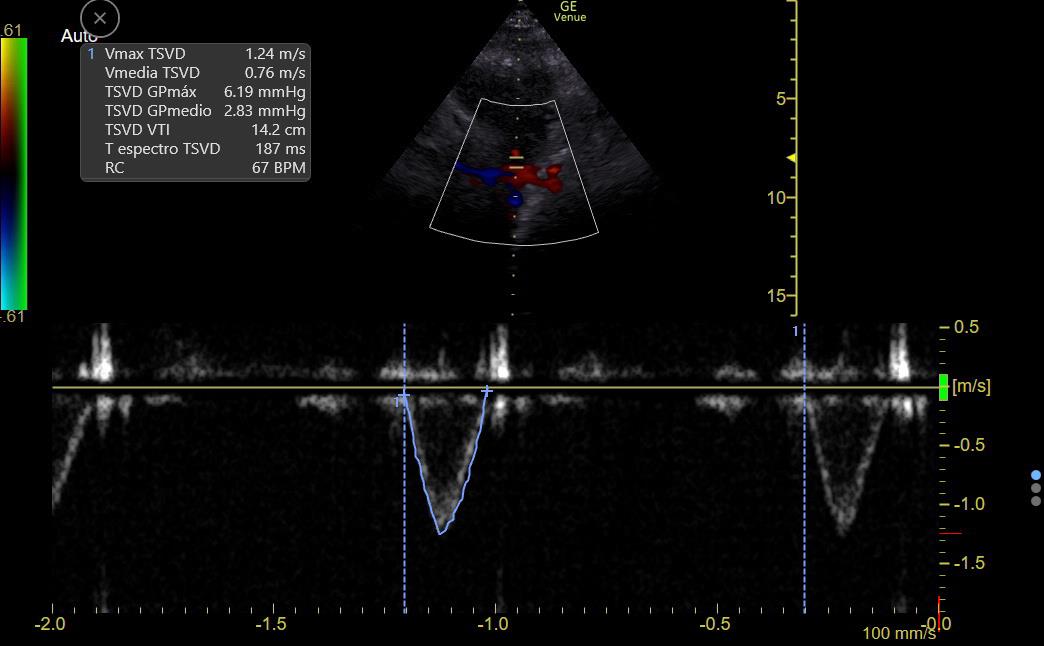
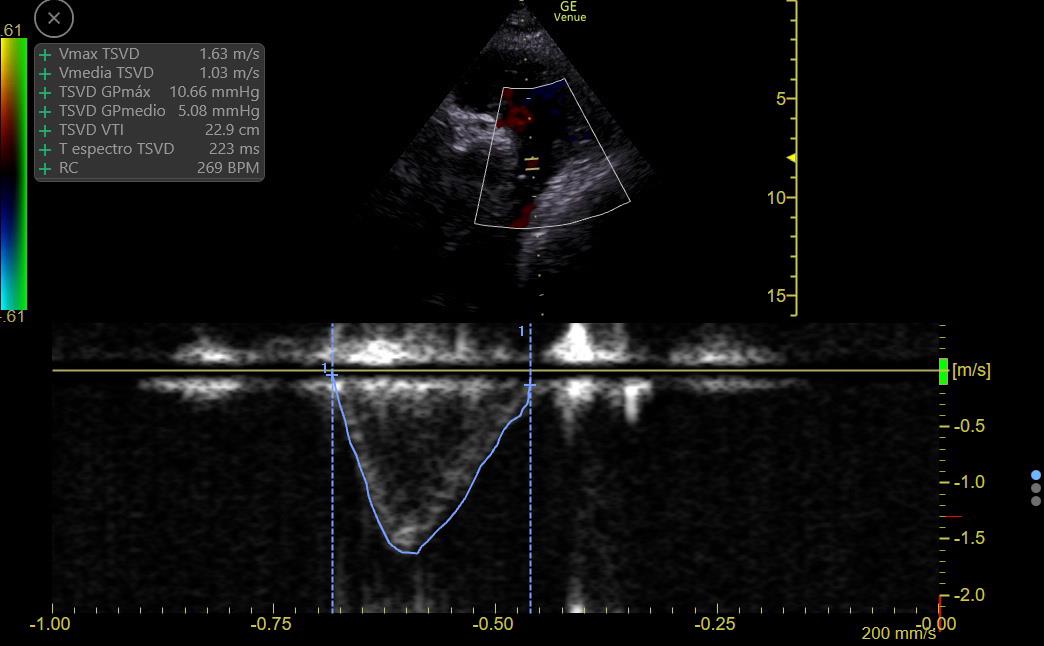
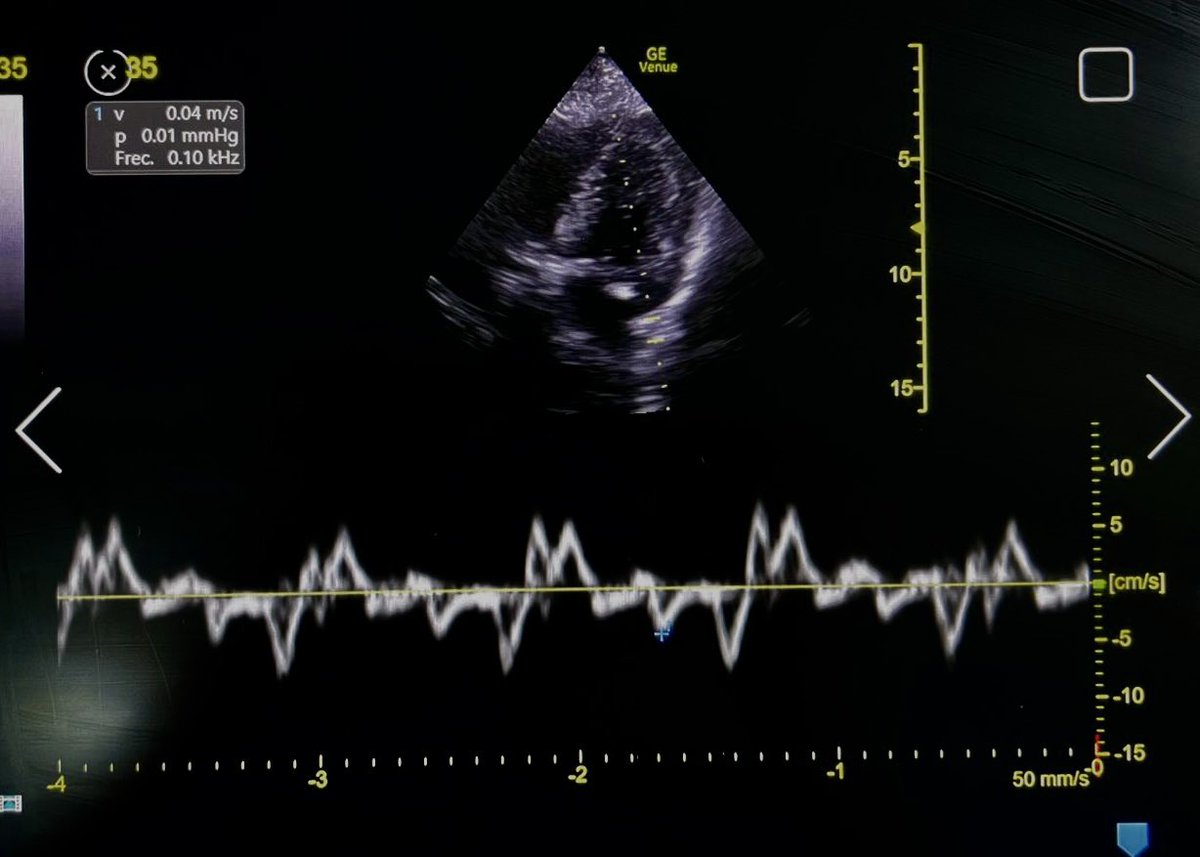
CO can be estimated by measuring flow at the LV or RV outflow tract:
RVOT Doppler shows ⬇️ VTI (9 to 14), so CO is LOW
There is ⬆️ respiratory variation: Low preload vs RV failure or Interdependence (Both Ruled out on #echofirst)
This suggests a low preload state
7/11
RVOT Doppler shows ⬇️ VTI (9 to 14), so CO is LOW
There is ⬆️ respiratory variation: Low preload vs RV failure or Interdependence (Both Ruled out on #echofirst)
This suggests a low preload state
7/11
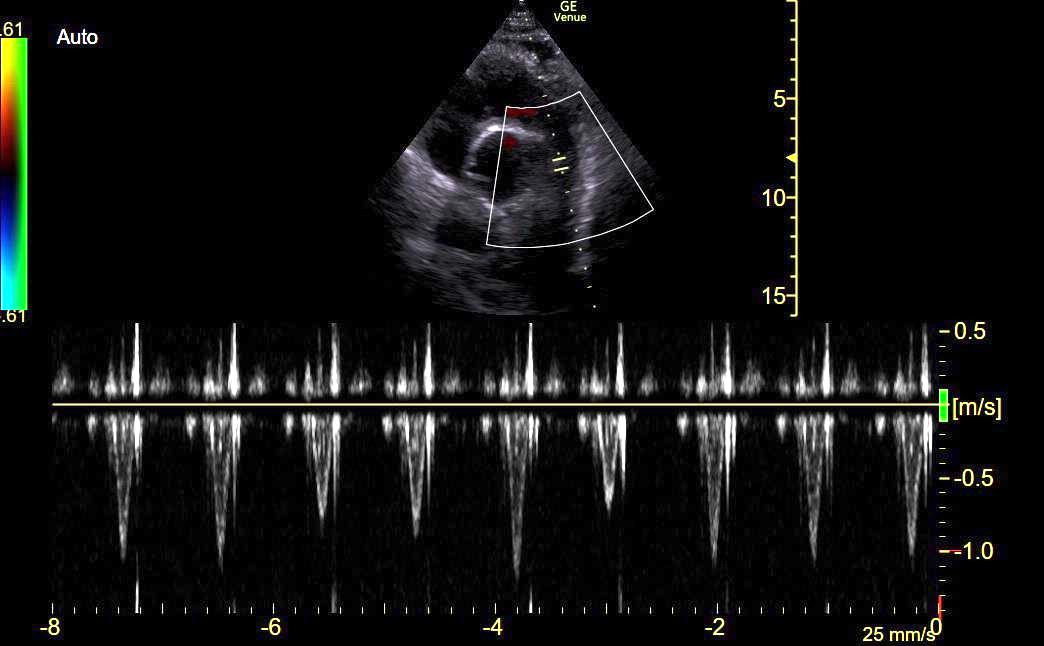
Plethoric IVC is likely due to IMV, this patient has low preload!
⬇️ preload can be caused by sepsis (venodilation/3rd spacing) or hypovolemia
#EchoFirst can't distinguish between these!
So, before giving fluid, it is wise to look for fluid tolerance 👇
8/11
⬇️ preload can be caused by sepsis (venodilation/3rd spacing) or hypovolemia
#EchoFirst can't distinguish between these!
So, before giving fluid, it is wise to look for fluid tolerance 👇
8/11
Why tweet about it?
I think it's a good example of all the reasoning that should go into evaluating hemodynamic AKI
#POCUS does not evaluate "Fluid Status"
Fluid status can only be determined by integrating the clinical context with a solid understanding of hemodynamics
/END
I think it's a good example of all the reasoning that should go into evaluating hemodynamic AKI
#POCUS does not evaluate "Fluid Status"
Fluid status can only be determined by integrating the clinical context with a solid understanding of hemodynamics
/END
جاري تحميل الاقتراحات...